Diabetics greatly benefit from short bursts of high intensity exercise
A group of diabetics lost 18 per cent belly fat and improved their sugar regulation, after just 8-weeks of short but high intensity exercise sessions. No drug has the same effect.
When a group of type-2 diabetic patients took part in an eight week program of high-intensity training three times a week, they experienced a huge reduction in their abdominal fat, improved glucose tolerance, and more active beta cells that make insulin in the pancreas.
These are the results of new research published in the scientific journal PLOS ONE.
"We find extremely large effects on a whole range of problems associated with diabetes. It‘s a pioneering study of a form of exercise that people actually find time to do," says co-author Per Bendix Jeppesen from the Department of Clinical Medicine at Aarhus University.
"We could hardly recognise them when they came to be measured the final time. Their fat distribution was quite different. One of the participants had lost 1.6 kilograms of belly fat in just eight weeks," he says.

"We have no medicine that provides the same powerful effect as this," says Jeppesen.
An affordable type of exercise
For the new study, researchers recruited 10 type-2 diabetics aged 56 to 58. They were all overweight with a BMI greater than 30 and did no regular exercise.
The scientists also selected 13 non-diabetic individuals, who otherwise had the same characteristics as the diabetic group, including age, weight, and level of physical inactivity.
Before the study started, the scientists measured participants’ glucose tolerance, the efficiency of their insulin-producing cells, and their abdominal fat.
Participants met at the gym three times a week, where they completed ten minutes of high intensity exercise--one-minute cycling and one-minute rest, repeated 10 times.
"This is something you can do at home and it takes half an hour, three times a week, so it’s manageable for most people," says lead author, Søren Møller Madsen, from the Department of Clinical Medicine at Aarhus University, Denmark.
Each practice session lasted 30 minutes, including warm up and cool down. During the rest intervals, participants could either rest completely or continue cycling at a low speed.
Large reductions in dangerous belly fat
After eight weeks of training, they re-measured the participants’ belly fat, alpha cell activity, and sugar tolerance.
The diabetic group had lost on average 18 per cent of belly fat, while the healthy group had lost 10 per cent. Belly fat is considered dangerous as it often leads to cardiovascular problems, which indicates that there is fat around the internal organs such as the liver and kidneys.
The big difference between the two groups can be explained by the fact that diabetics generally have more abdominal fat than the healthy group. But the difference between the groups, as well as the amount of abdominal fat lost after just 8 weeks, surprised the scientists.
Better sugar regulation and improved insulin production
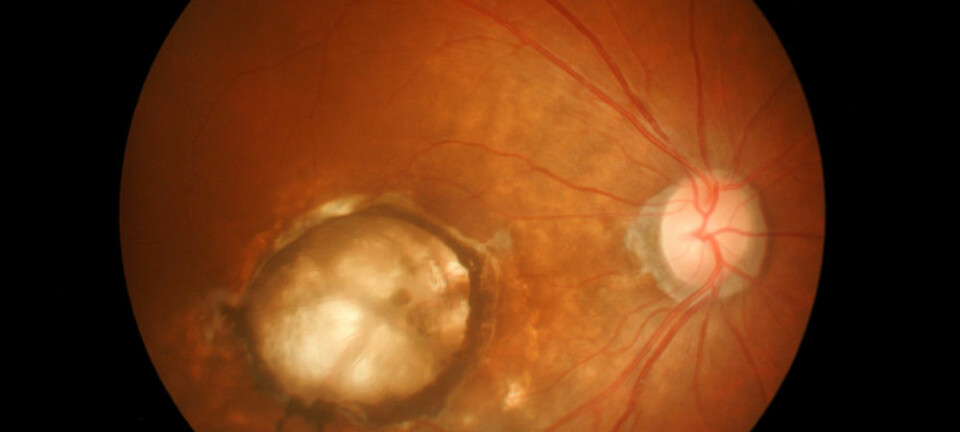
Participants with diabetes also improved their sugar tolerance by 12 per cent. That means their blood sugar levels dropped 12 per cent after consuming glucose, compared to the initial tests.
The diabetics’ insulin producing beta cells also become more sensitive to glucose.
"The problem for diabetics is that their beta cells do not register the sugar and therefore do not produce enough insulin to break it down. But after the 8-week training program, the beta cells responded faster, so they can identify the sugar faster and start producing insulin," says Jeppesen.
All of participants improved their lung capacity and their blood pressure was noticeably lowered.
Very hard training for diabetes
According to Mathias Reid-Larsen, postdoc at the National Centre for Health at the National Hospital, Denmark, the new results are very interesting. He thinks that his form of exercise could be accessible to people with weight problems that may not otherwise take part in exercise, as well as diabetic patients.
"The most impressive thing is that 100 per cent of the participants show up throughout the study,” says Reid-Larsen.
Earlier studies have shown that 80 per cent of patients with type-2 diabetes do not maintain physical activity. But this type of training may be a good model for encouraging patients to exercise, and to keep it up.
All participants took part in the training until the end--despite the fact that it was very strenuous.
"It was very hard. People thought the training was mentally tough, but they had a coach who motivated them a lot. It also helped that they could sense a physical change happening," says Madsen.
Reid-Larsen suggests it would be interesting to compare these results with an alternative study where people could train at home without a motivational coach.
"The next step is to do the same experiment with a larger group and to have a control group--a group of diabetics with no coach. It would also be exciting to see how it works over longer periods,” he says.
Reid-Larsen is interested to see if this 100 per cent attendance record can be repeated in an exercise program that lasts longer than 8 weeks, or in a home based program with no coach.
---------------
Read the Danish version of this article on Videnskab.dk
Translated by: Catherine Jex