Human organs-on-chips may one day replace animal testing
Scientists have developed more than ten different human organ chips, including devices to mimic critical functions of the lungs, kidneys, intestines, liver, and bone marrow. Eventually this technology could render animal testing obsolete.
The drug development model is broken. This is the conclusion that I have reached after 30 years as an academic researcher in medicine.
The amount of funding funnelled into medical research and drug development has increased dramatically over the past fifty years. And yet the number of new drugs that successfully pass through human clinical trials and receive regulatory approval has decreased steadily over the same period, when the increasing level of research and development investment is taken into account.
It currently costs more than US$2.6 billion to move a drug from discovery at the bench through regulatory approval, and the reality is that most drugs fail at the most expensive later phases of human clinical testing. Thus, the pharmaceutical industry’s new mantra is to “fail quickly and cheaply”, which to a scientist like myself, is no vision at all.
There are many reasons why the current drug development model is broken, however, one of the major problems is that animal testing, which is required for regulatory approval and can take years to complete, often does not predict clinical responses in humans.
Thus, when we founded the Wyss Institute, I focused one of our major platforms on this problem of developing alternatives to animal testing in order to accelerate drug development, and potentially to create a new approach to personalized medicine as well.
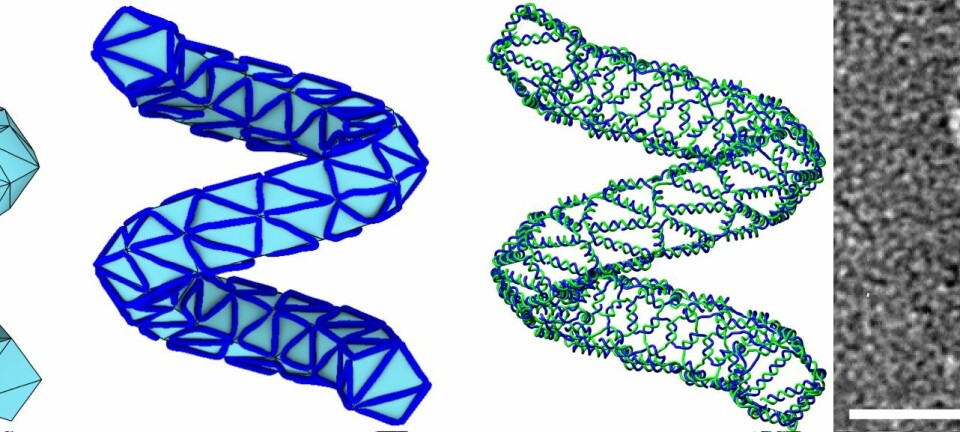
Engineered microchips with living human cells
The approach we pursued is to engineer microchips containing living human cells that reconstitute organ-level functions outside the body, and to create what we call ‘Organs-on-Chips’.
You might ask, “why microchips?”.
Well, the manufacturing methods developed to make computer microchips offer control of features at the same nanometer to micrometer size scale of living cells and tissues.
We do not actually culture cells directly on the computer chips; instead, we use these methods to create molds that allow us to fabricate micro-devices with hollow channels (essentially artificial microvascular networks) in which we culture cells and flow life-sustaining fluids.
Read More: 3-D printed organs may solve organ donation shortages
Success with a Lung-on-a-chip
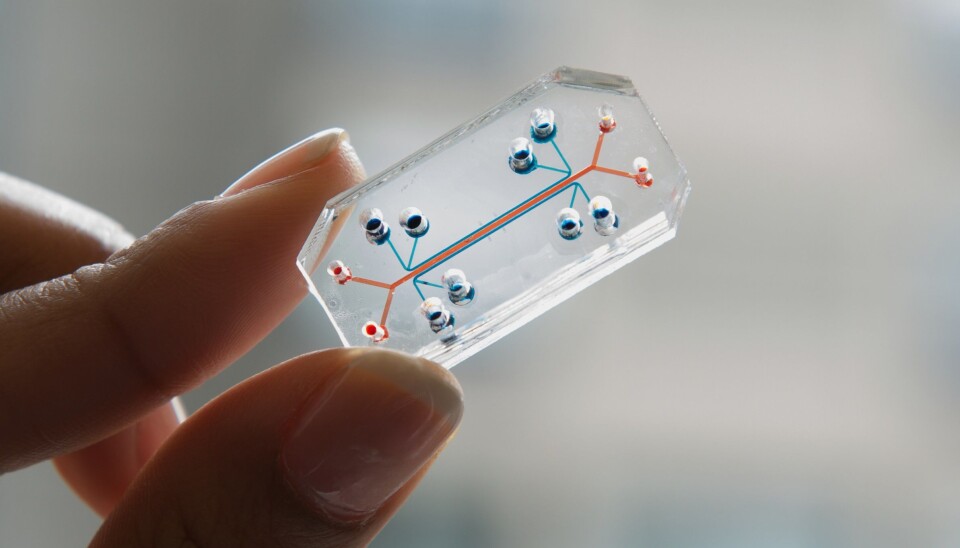
Our first success involved the development of a human breathing lung-on-a-chip that reconstituted the structure and function of the air sacs of the lung. This lung chip is about the size of a memory stick and is composed of a crystal clear, flexible, polymer that contains three parallel microchannels.
The central microchannel is split into smaller top and bottom channels by a thin, flexible, porous membrane that is lined on its top side with human lung cells from the air sac and exposed to air.
Human capillary blood cells are placed on the bottom side of the same membrane with medium flowing over their surface within the lower channel to mimic blood.
A vacuum applied to the side channels deforms this tissue-tissue interface to recreate the way lung tissues physically expand and retract when breathing in the whole human lung.
This simple human lung chip is able to mimic many complex functions of the living lung organ, including inflammation caused by contact with smog particulates or infectious bacteria.
You can see how this chip works in the video below.
We also used the human lung chip to mimic diseases, such as pulmonary edema or ‘fluid on the lungs,’ and to discover drugs that prevent this condition.
We even gained new insights into how our organs work because we can control and vary all of the individual cells and components added to these devices. For example, we discovered that physiological breathing motions influence absorption of smog particulates, as well as drug toxicities.
Most recently, we extended this work by creating lung chips with small airway cells from human patients with chronic obstructive pulmonary disease (COPD), and when we exposed them to cigarette smoke, they displayed the same heightened sensitivity in terms of smoke-induced injury and inflammation as seen in human COPD patients.
A human breathing lung-on-a-chip replicates the structure and function of the air sacs of the lung. A central microchannel is split into two channels by a thin, flexible, porous membrane lined with human lung cells (top) and human capillary blood cells (bottom). A vacuum applied to the side channels recreates the way human lung tissues physically expand and retract when breathing. (Video: Wyss Institute at Harvard University)
Started to create a ‘Human Body-on-chips’
Over the past six years, we have developed more than ten different human organ chips, including devices that mimic critical functions of the lungs, kidneys, intestines, liver, and bone marrow, among others, and we have modelled other human diseases, such as inflammatory bowel disease (IBD), as well as drug toxicities.
We have also cultured living microbes from the human microbiome for weeks in direct contact with living intestinal cells within our human gut chip, which opens up a new path to study how the microbiome influences human health and disease.
But we have gone even further--we have begun to create a ‘Human Body-on-chips’ composed of multiple human organ chips sustained as integrated system by transferring fluids between their blood vessel cell-lined vascular channels.
The goal here is to use this model to determine the dynamics of drug absorption, clearance and breakdown, as well as drug effects on target tissues, so that we might be able to determine appropriate doses to use in human trials without requiring animal testing.
However, the same approach could also be used to test for dangerous effects of environmental toxins, cosmetics, household chemicals or any other environment factor.
Read More: 3D-printed organs give insights to complex anatomy
Personalised medicine on the way?
Another exciting line of future research is the use of human organ chips for personalised medicine.
Given recent advances in stem cell technology where virtually any tissue type can be generated from adult skin or blood cells, someday we might be able to make your lung chip and test drugs to determine which is the best drug for you.
Or we could make organ chips from patients that represent different ethnic groups or genetic subpopulations.
We could even imagine making chips with cells from children to overcome the huge challenge we face today in terms of carrying out clinical trials in paediatric populations.
Read More: What are the major challenges to modern medicine?
A game-changer in medicine
I believe that combining stem cell technology with human organ chips will represent an even bigger game changer that goes far beyond personalised medicine.
The reality today is that major pharmaceutical and biotechnology companies spend huge sums to move drugs into clinical trials, and they often fail. They then analyse the data generated to explore whether some genetic subgroup of patients might have responded better than others.
If they are lucky, these companies then initiate a much more focused trial with that sub-population, and if successful, they obtain approval for a much narrower clinical application, but at great expense.
In a future with organ chips, you can imagine generating lung cells from a particular patient subgroup--say middle-aged Hispanic women with a history of COPD who are highly sensitive to cigarette smoke.
We can then make lung chips from those patients, test drugs on those chips and then use that same cohort of patients for a focused human clinical trial. This approach could drastically shorten the time required for drug development, greatly reduce costs, and significantly increase the likelihood of success.
The promise is great, but the challenge is huge.
While we cannot expect these devices to replace animal testing in the near future, if all goes well, we will see one animal model replaced at a time as data are generated that confirm chips lined with human cells can be equally robust as animal models, but produce even more relevant and predictive results.