Tapeworm parasites in the brain give epilepsy
Traces of pork tapeworm that end up in the human brain can cause epilepsy, but both the parasite and its complications in the form of disease can be fought.
Twenty-one-year-old Isabel grew up in the countryside near Maputo in Mozambique. She’s a pretty woman, went to school for six years and comes from a good family.
But her chances of marrying and getting children are slim – because Isabel has epilepsy, a brain disorder characterised by repeated seizures (convulsions); seizures are episodes of disturbed brain activity that cause changes in attention or behaviour.
Comes from excrement
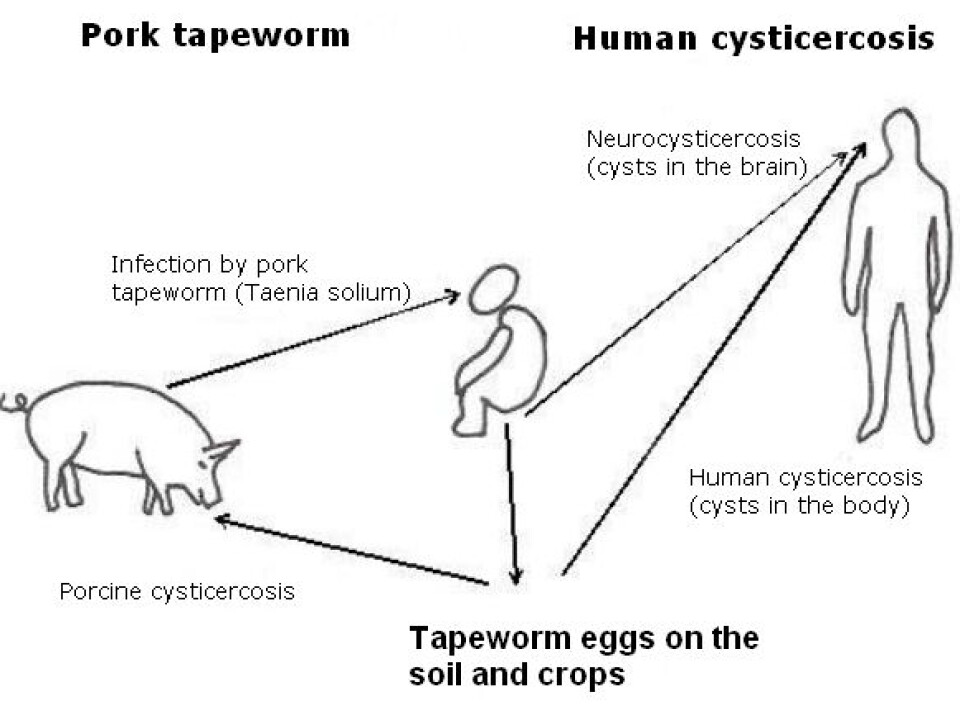
Isabel developed epilepsy because she happened to eat eggs from a tapeworm in human excrement – from a family member, friends or neighbours. The tapeworm eggs had developed into cysts (sacs containing the tapeworm larva) in her brain.
Isabel’s village has no flushing toilets, and not everyone uses the latrines that have been dug. Instead, Isabel and other villagers retire behind a bush when they need to go to the toilet while working in the fields or on their way to or from the market or school.
This means that the tapeworm’s eggs are found on plants or in the soil, where they can be eaten by pigs or even by people. When the tapeworm’s eggs develop in the body of a human or a pig, the human or pig develops a disease called cysticercosis.
Undercooked pork can also infect you
Humans and pigs with cysticercosis have cysts in their bodies. While this disease results in few significant symptoms in pigs, the cysts will often end in humans’ brains, which a large amount of blood flows through. Cysts in the brain cause neurocysticercosis.
From the parasite’s point of view, humans with cysts in their brains or bodies are a dead-end development – the parasite cannot reproduce itself. But if tapeworm eggs or larva reach a human’s intestines, because the human has eaten undercooked pork infected by tapeworm cysts, the tapeworm can reproduce itself.
Cysts and epilepsy
Scientists at the University of Copenhagen’s Department of Veterinary Disease Biology have been involved in researching cysticercosis and have been supervisors for several PhD students from Africa.

One of the scientists, Maria Vang Johansen, a veterinary surgeon and a professor at the department’s Section of Parasitology, Health and Development, says the connection between cysticercosis and epilepsy is extremely well documented.
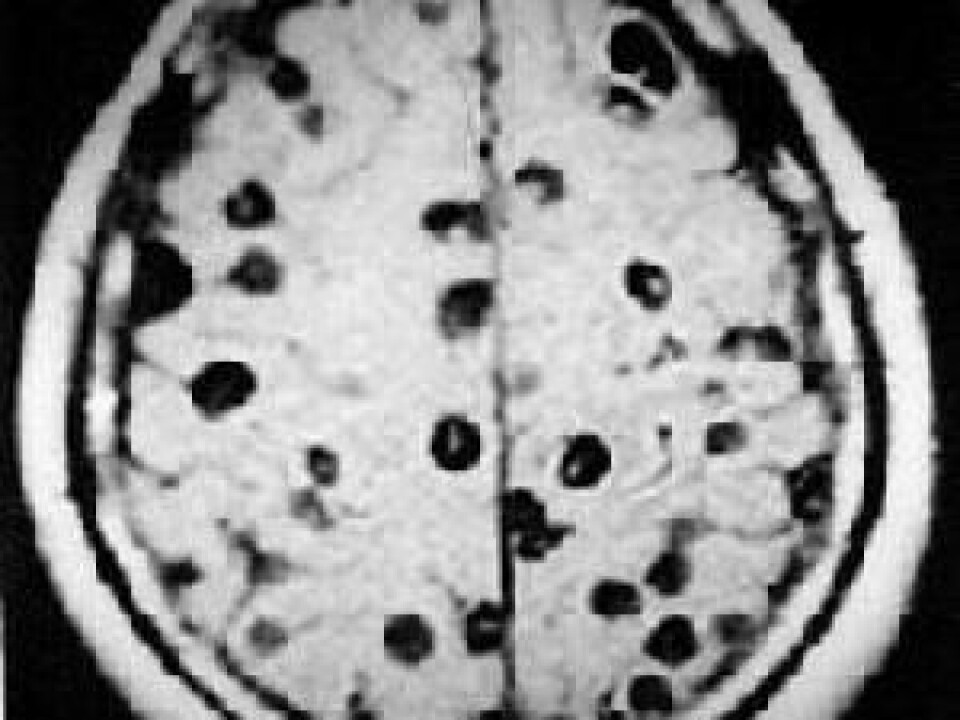
Researchers who scan the brain of an epilepsy patient very often find both parasite-specific antigens circulating in the patient’s blood – which documents the existence of living parasites – and spherical bodies up to 1 cm in size in the brain.
Cysticercosis never gives an unambiguous picture
“A picture will never be 100 percent unambiguous,” says Johansen when asked whether the spheres in the brain could be caused by something other than cysticercosis. “But we can see either clearly limited sclerosis, which are dead cysts, or lesions with active cysts,” she adds. “The active cysts are seen as circular, limited concentrations, which are very good indications of brain cysts, but we can never completely preclude that they could be something else.”
However, by assessing the size and form of the concentrations, the researchers can often determine that they are cysts. But the location of the cysts cannot be used to determine their existence – they are found in all parts of the brain.
Epilepsy caused by cysts can be treated
Now that researchers have shown a connection between the parasite and epilepsy, can the epileptic patients be treated?
Johansen says the answer is yes, but the treatment must be very intensive: hospitalisation with anthelmintic medicine (which is active against parasitic worms), and treatment against both epilepsy and inflammation, plus possible standard treatment with fluids should the patient go into medical shock.
“We believe that treatment with anthelmintic medicine increases the risk of an epileptic seizure, because the dead cysts will release the antigen that triggers a reaction from the patient’s immune system, and it’s this reaction, which is inflammatory, that causes the epileptic seizure,” she says.
Prevention is the key
This treatment, however, not only requires a well-functioning hospital, but is also only possible for a very small proportion of the people affected. Other measures are needed.
“Prevention, prevention and prevention,” is how Johansen describes the best way of ensuring that fewer people develop cysticercosis and thus risk getting epilepsy.
Local health authorities must tell the villagers how epilepsy arises. The villagers don’t know the origin of epilepsy and believe it is due to a curse on them – and they go to traditional healers, medicine men or witch doctors to resolve this situation, not to trained medical staff to treat the disease.
As a disease, epilepsy is taboo and its sufferers are stigmatised and kept out of sight; sufferers find it difficult to get work and marry.
“Our aim must be to get the villagers to despise how they treat sufferers and take responsibility for their actions,” says Johansen. “They must understand that if they relieve themselves behind a bush, rather than use the latrines, they, their family or neighbours risk eating the excrement and any tapeworm eggs either on crops or in pork.”
--------------------------------------------------
Read this article in Danish at videnskab.dk
Translated by: Michael de Laine
Scientific links
- A Cross-Sectional Study of People with Epilepsy and Neurocysticercosis in Tanzania: Clinical Characteristics and Diagnostic Approaches; PLoS Negl Trop Dis 5(6): e1185. doi:10.1371/journal.pntd.0001185
- García, HH, Gonzalez, AE, Evans, CAW, Gilman, RH. (2003). Taenia solium cysticercosis. Lancet, 361, 547-556
External links
- Maria Vang Johansen's profile
- Annette Olsen's profile
- About tapeworm infections (NHS)
- About Epilepsy (PubMed Health)