Bestseller drug may cause osteoporosis
The world’s second-most common prescription drug, Plavix, may increase the risk of osteoporosis, new study reveals.
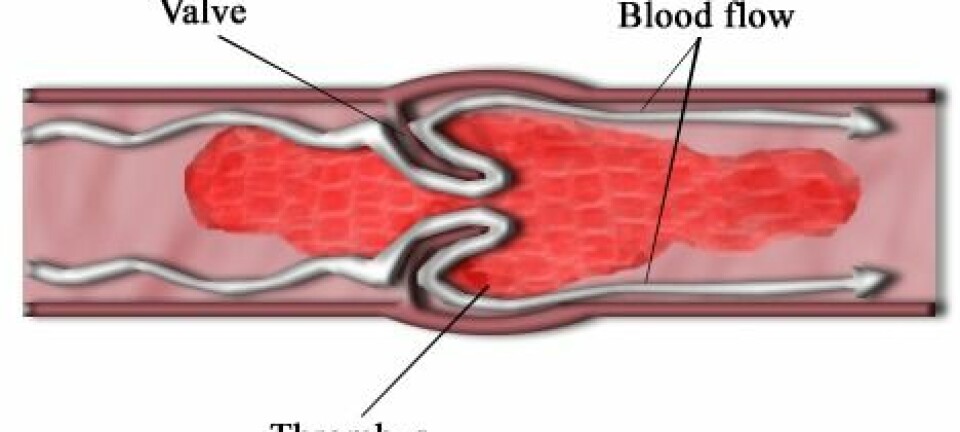
A comprehensive new study indicates that the world’s most widely used drug to treat blood clots and heart disease has a serious and completely overlooked side effect.
The drug marketed as Plavix is prescribed to millions of people in numerous countries around the world because it is believed to work effectively without major side effects.
But now Danish researchers surprisingly conclude that the blood-thinning drug may increase the risk of patients developing osteoporosis – also known as brittle bone disease – and thus risk breaking e.g. their spine, hips or wrists.
”It appears that the risk of developing osteoporosis increases by around 50 percent, primarily for people who have been taking the drug for a year or longer,” says Niklas Rye Jørgensen, chief physician at Glostrup Hospital.

“This is interesting because Plavix has been a ‘blockbuster drug’ for some years now, where it’s been number one and two on the list of best-selling drugs in the world, so many people are affected. And the harmful effect may be quite considerable.”
More than 300,000 participants
Together with Danish and international colleagues, Jørgensen has examined 77,000 Danish patients, who in the period 1998-2008 were treated with Plavix or other drugs which, like Plavix, contain the active substance clopidogrel.
The researchers have via the Danish Civil Registration System found the number of osteoporosis cases among these patients and compared them with a control group of 230,000 Danes who did not take clopidogrel.
After having adjusted for other factors that may affect the risk of osteoporosis, the researchers were left with something that looks like a clear conclusion: patients on clopidogrel have a far greater incidence of broken hips and wrists as well as spinal collapse than those who have never taken clopidogrel.
It’s extremely important that patients keep taking the drug. Clopidogrel significantly reduces the risk of getting a new blood clot, especially for patients in life-long treatment following a brain clot. In my opinion, dropping the drug is far more damaging than if you develop osteoporosis, so they must for God’s sake not stop taking it.
Niklas Rye Jørgensen
The new study is published in the Journal of Internal Medicine.
No proof that clopidogrel causes osteoporosis
Although the study indicates a significantly increased risk, Jørgensen notes that the study does not establish a clear cause. Factors not taken into account in the study include measurements of the patients’ bones before and after taking clopidogrel, calcium contents in each individual and their lifestyles or physical condition. And who knows – perhaps patients on clipodogrel are generally frail people whose bones would break more easily even without taking the drug?
The research team therefore concludes that it is indeed likely that there’s a correlation between clopidogrel and osteoporosis, but also that it’s too early for any certainty.
“This provides us with some hypotheses around the link between clopidogrel and the risk of developing fractures, and we will continue working with these hypotheses. But more direct examinations of the potentially harmful effects of taking clopidogrel for the individual is a topic for upcoming studies,” says Jørgensen.
Warning: do not stop taking the drug!
In the very same breath, the researcher sends out a strong warning to patients who believe that they now have to stop taking Plavix because they want to avoid the potentially great risk of developing osteoporosis.
“It’s extremely important that patients keep taking the drug. Clopidogrel significantly reduces the risk of getting a new blood clot, especially for patients in lifelong treatment following a brain clot. In my opinion, dropping the drug is far more damaging than if you develop osteoporosis, so they must for God’s sake not stop taking it.”
Thorough experiments with Plavix coming up
The next step is to design an experiment that gives a reliable indication of how clopidogrel affects humans.
”We need set up a good old-fashioned clinical trial in which one group receives the drug while another does not. It has to be a parallel study conducted on the same type of patients, where we monitor their bone status over the year or two they’re taking part in the study,” says the researcher.
The problem, however, is that Plavix is the standard treatment for patients with blood clots and heart disease, so it’s not responsible to ask a group to stay away from the treatment to see if they develop osteoporosis.
Cerebral haemorrhage patients can help blood clot patients
With a little luck, the solution to this problem may well be found within the walls of Glostrup Hospital. Here they do not only treat patients with brain clots, but also those with cerebral haemorrhages.
These two patient groups are quite similar, but whereas a brain clot is treated with blood-thinning drugs, treating a cerebral haemorrhage with such drugs would only make matters worse. This is why patients with cerebral haemorrhage are never given clopidogrel.
Comparing the bones and the contents of e.g. calcium and minerals, along with each individual’s risk of developing osteoporosis in these two similar patient groups, might lead to conclusive answers about whether or not clopidogrel damages human bones. This would also make it easier to come up with recommendations on how to avoid the unpleasant side effect.
The researchers are currently applying for funding for the follow-up study. If successful, Jørgensen and his colleagues expect to come up with a clearer conclusion within a couple of years.
--------------------------------
Read the Danish version of this article at videnskab.dk
Translated by: Dann Vinther
Scientific links
- "Clopidogrel and the risk of osteoporotic fractures: a nationwide cohort study", Journal of Internal Medicine; DOI: 10.1111/j.1365-2796.2012.02535.x
- "Clopidogrel (Plavix), a P2Y12 Receptor Antagonist, Inhibits Bone Cell Function In Vitro and Decreases Trabecular Bone In Vivo; Journal of Bone and Mineral Research", DOI: 10.1002/jbmr.1690