Many men needlessly tested for prostate cancer
Doctors often retest men for prostate cancer, even though the first test showed no signs of cancer. This is pointless and debases male patients, say scientists.
Anxiety, infections, and life-threatening blood poisoning. These are some of the possible consequences that can occur from the biopsy taken when testing men for prostate cancer.
A new study finds that the negative impact of needlessly taking more than one biopsy can be so big that it should be avoided all together.
“In the world’s largest study ever, we show that if the first biopsy is negative, then the probability of dying from cancer is very, very low. The risk must be balanced against the risk of eventually dying from something else and the unpleasantness that comes with the test,” says Andreas Røder, a doctor at the Copenhagen Prostate Cancer Center (CPC) at Rigshospitalet, Copenhagen University Hospital, Denmark, and the supervisor of the study.
The study was prepared by the CPC in cooperation with the Department of Pathology, Rigshospitalet. It is based on data from 64,000 Danish men who have been under examined for prostate cancer between 1995 and 2011.
The new results are published in the Annals of Oncology.
One biopsy is enough
The prostate is a gland that sits just where the bladder meets the urethra. Indications of prostate cancer can include blood in semen or urine.
A blood test can analyse for PSA numbers, that is, how much prostate-specific antigen is contained in the blood. A higher PSA number is indicative of cancer.
“Men who have a PSA number under four have a very low risk of prostate cancer, and so we don’t do any further tests,” says lead-author Nina Klemann, a doctor at CPC.
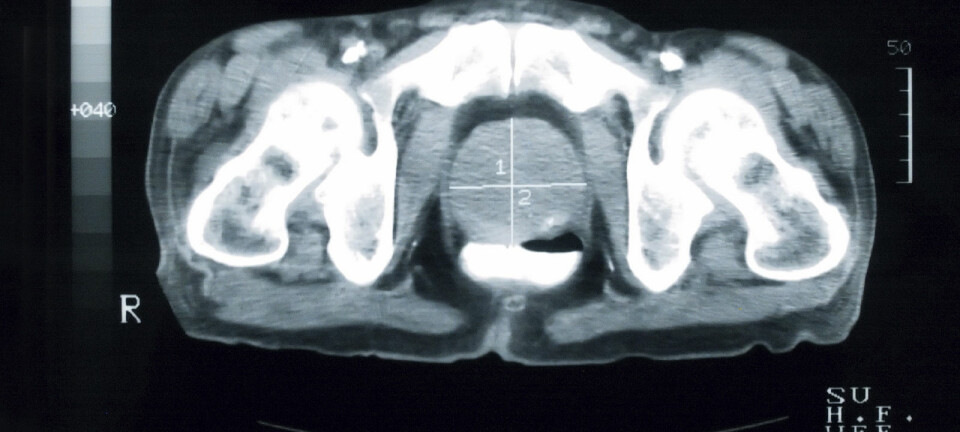
Men who have a PSA number over four are referred for a biopsy where a tissue sample is taken via the rectum.
But some patients are sent for another biopsy, even if the first biopsy is negative.
It is completely unnecessary, says Klemann.
"A little over 27,000 of the 64,000 men registered had negative biopsies. Out of them, two percent, or approximately 500 men will eventually die of prostate cancer,” says Klemann.
“In this case, we believe that it’s unacceptable,” she says.
It is important to offset the negative impact of the biopsy against how many lives are actually saved by multiple tests, says Klemann.
Read More: Football saves the bones of prostate cancer patients
Scientists are skeptical of fewer tests
Michael Borre, a professor and research scientist in prostate cancer at Aarhus University, Denmark, is skeptical of the study’s conclusions.
He acknowledges that biopsies can have unpleasant side effects, but this does not outweigh the prospect of saving more lives, he says.
“It’s a well-known risk that biopsies can cause blood poisoning. But if you can save more, I don’t necessarily mean that you have to omit several biopsies,” says Borre.
Techniques used in diagnosing prostate cancer are changing rapidly, he says. For example, patients may be sent for an MRI-scan following an initial negative biopsy.
“I think we should look at Norway and Sweden, both of whom have introduced MRI scans, which are much more precise in determining whether there’s cancer. That way you can find out who has the dangerous prostate cancer and who can be sent home with peace of mind,” says Borre.
Read More: How hereditary is prostate cancer?
Test erodes quality of life
The scientists behind the new study also believe new methods are needed to diagnose prostate cancer.
However, multiple biopsies are not the solution, even if it can save lives, says Klemann. It simply doesn’t outweigh the painful and risky side effects, she says.
“A biopsy is done with a needle through the rectum, and it can cause inflammation and bleeding. A very small few actually die of it,” she says.
A biopsy of the prostate can have some serious side-effects in otherwise healthy men, such as bleeding, pain and risk of infection, and it can ultimately lead to treatment related side-effects such as impotence and incontinence.
“It can reduce the life quality in healthy men, which is significant if it is unnecessary,” says Røder.
————————
Read the Danish version of this story on Videnskab.dk
Translated by: Catherine Jex