
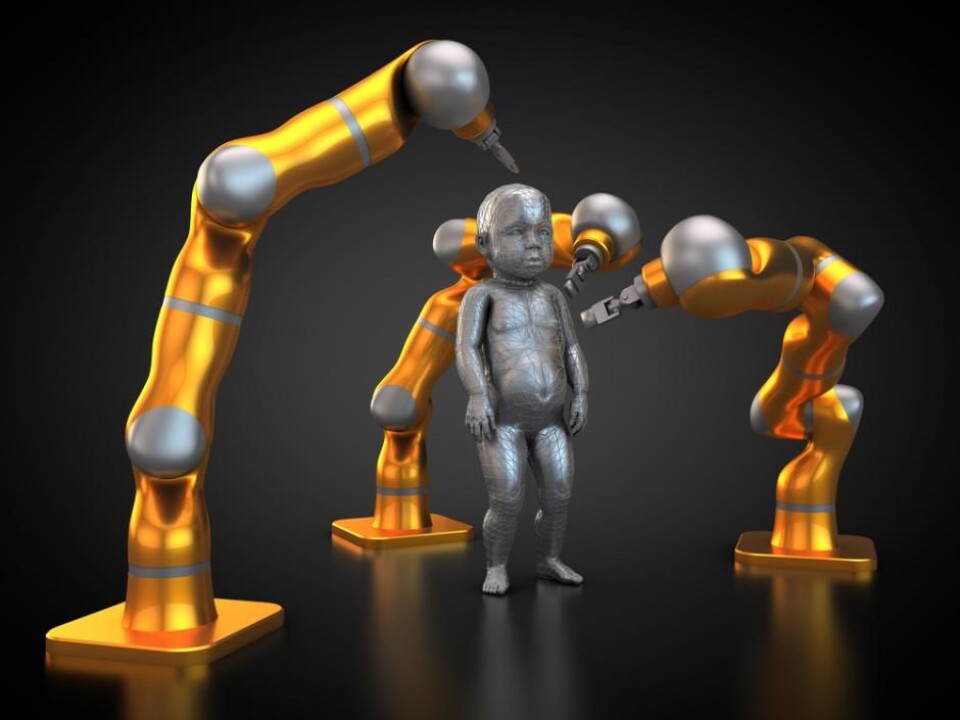
Genome editing: Are we opening a back door to eugenics?
We need to talk about the ethical aspects of CRISPR to control where we go from here.
Genome editing has been largely applied to animals and plants, but it now includes people. Who will decide what the technology will be used for and how far we should take it?
Philosophers, theologians, and sociologists, have debated fiercely for years about the ethical and social consequences of removing the disposition for certain diseases in unborn children by intervening with the sex cells (egg and semen) or the fertilised egg (the embryo).
It is still illegal to genetically modify human embryos in Denmark and Germany, but will the introduction of CRISPR/Cas9 change attitudes?
The same question applies to genetic enhancement that would change the properties of healthy embryos.
Read More: CRISPR breakthrough ignites hope of using pigs as organ donors
A game-changer in genome editing

Theoretical discussions about the social and ethical implications of future genetic enhancement has often been rejected outright by natural scientists as speculative thinking, completely dissociated from feasible or probable developments in science. But recently, the situation has changed.
Many scientists perceive CRISPR/Cas9 as a game-changer, allowing them to intervene in the human genome in a number of ways.
The technology is marketed as more flexible, precise, cheaper, and easier to use than existing techniques, such as TALEN and ZFN.
It allows scientists to remove, insert, or change the DNA sequences virtually anywhere in the genome. In principle, we can make a number of modifications simultaneously in a single genome, which presents opportunities to treat complex diseases or to change certain traits.
Read More: Scientists close to a cure for sickle cell anaemia
We need an open discussion about the technology
A number of leading biologists in the USA, including David Baltimore from the California Institute of Technology, USA, called for a discussion about the responsible use of the technology in 2015, following rapids developments in genome editing.
Writing in Science, he argued that before implementing the technology, we need to address the social, environmental, and ethical implications of inherited genetic modifications, which could be passed on to subsequent generations—so-called germline modification.
However, the question of how to balance current interventions with possible future consequences, should not be decided behind closed doors by the research community. It should be an open discussion with scientists from many fields, industrial partners, health authorities, legal advisers, lawyers, and the wider public.
Baltimore and his colleagues questioned the circumstances in which we could make responsible use of human germline modifications, in order to treat or cure human diseases. Is it appropriate to use the technology to change a disease-causing genetic mutation to a sequence more typical among healthy people?
How can we guarantee that we will not unintentionally change other genes (so-called off-target effects) given our limited knowledge of human genetics, gene-environment interactions, and disease occurrence or progress (for example, the interaction between one disease with another condition in the same patient)?
How can we avoid inflicting more harm than good on future humans with our current, limited state of knowledge? Baltimore’s group suggested that research be put on hold until these questions had been addressed.
Read More: Scientists want to collect your DNA when you die
Chinese research led the way
Others were opposed to germline modifications, because they feared that even the permission to conduct laboratory research on embryos at the earliest stages of development, in the hope of creating future therapeutic interventions, could be a slippery slope towards the production of so-called designer babies and the enhancement of humans.
In their view, that could lead to a liberal eugenics, where parents make independent decisions about their children’s genes.
While Baltimore’s group urged restraint, scientists on the other side of the world took a different view. That same year, scientists in China published two articles describing advances in CRISPR/Cas 9 technology applied to human embryos (the embryos were later destroyed in compliance with Chinese ethical guidelines).
Despite loud protests from other scientists and members of the public around the world, the research spread to Sweden, the UK, and the U.S.
Read More: Genetic test queues generated by Angelina Jolie
UK Embryo studies with CRISPR
On the 20th September 2017, Nature published a research article describing how a team of scientists in the UK from the Francis Crick Institute, London, under the leadership of Dr. Kathy Niakan, had be granted permission to edit the genome of a human embryo to study the role of genetics in the earliest stages of development.
Using CRISPR/Cas9, they deactivated a gene that coded for a protein by the name of OCT4 in zygotes (combined egg and semen). The study showed that embryos unable to produce OCT4 struggled to develop as they should.
According to Niakan, application of the precise CRISPR/Cas9 tool to human embryos gave them a unique insight and understanding of the genome’s function, which would not have been possible through studies of mice. In their opinion, continuing research on human embryos was extremely important.
Read More: Scientists are mapping the entire Danish genome
Ethical recommendations in Denmark, UK, and the U.S.
Since then genome editing technology has developed at such speed that it has become difficult to keep up with the ethical and social implications.
But in 2016, The Danish Council on Ethics released a report entitled ‘Opinion on genetic modification of future people.’ That same year, the Nuffield Council on Bioethics in the UK released a similar review: ‘Genome editing: an ethical review.”
And this year, the American National Academy of Science and the National Academy of Medicine followed suit with their report entitled ‘Human genome editing—science, ethics and governance.’
Continued tight regulation
Many people were surprised that the American report did not recommend a total ban on clinical trials of human germlines.
The report established that the technology could potentially be used to treat rare, dangerous diseases, if and when a long list of criteria could be met, which would ensure strict regulations and limit use to particularly dangerous cases.
But the authors acknowledge that some of the criteria are only vaguely defined. For example, they stipulate that clinical trials using germline editing with implications for future generations could only be allowed if there were no other reasonable alternatives, or in order to avoid dangerous diseases or conditions.
The decision of what constitutes ‘dangerous diseases or conditions’ could be interpreted in a number of ways according to specific historical, cultural, and social characteristics.
They also say that doctors and patients will typically conduct their own evaluation of which particular conditions characterise each individual case. Whether there are ‘reasonable alternatives’ must therefore be judged in each individual case.
These criteria could be interpreted in the strictest sense, making certain procedures impossible. Alternatively, they could be interpreted in a less restrictive way.
They also recommend close monitoring of the uses of the technology, to avoid it being used for anything other than fighting serious diseases. At the same time they acknowledge that it is difficult to make a sharp distinction between normal function and disease, treatments and genetic enhancement.
Read More: New European genome HQ to create genome atlas
Many unanswered questions
The US report is criticised for not taking a firm position on anything other than the ‘usual’ ethical questions concerning the distinction between treatment and enhancements and between normal functioning and disease.
Peter Mills, assistant director of the Nuffield Council on Bioethics and co-author of the council's report into the ethics of genome editing, wrote in a blog that the discussion should also include important questions about how the implementation of germline procedures will interact with current and future societal discourse, institutions, and law.
We must reflect thoroughly on how the technique might creep across distances, both functional and geographical.
Which existing techniques and treatments will be replaced by genome editing?
Which moral transformations will an expansion of genome editing potentially lead to, and how can we prevent or deal with any negative consequences?
The Danish report focussed on a range of ethical questions concerning the balance of risk, consideration of future children and parents, the right to an open future, equality and inequality, the impacts on nature and biodiversity, and implications for tolerance and acceptance of people who are perceived as different. But there was very little focus on the issues raised by Mills.
Read More: Scientists embark on the world’s largest genome project
Only ‘perfect’ people in the future?
It is not only philosophers, theologians, sociologists, and biologists that are concerned about the future ethical and social implications of CRISPR/Cas9.
Many people suffering from a number of physical and psychological illnesses and conditions are interested in the potential future opportunities to treat genetic diseases and prevent extremely severe conditions being passed on to their descendants.
But they also express concern over whether implementing the technology could cause a gradual change in public opinion and acceptance towards people suffering from genetic conditions and disabilities.
Are we heading towards a society where we strive for physical and psychological perfection? Or will society accept those who are, or choose to remain, ‘different?’
Read More: Human organs-on-chips may one day replace animal testing
Will children with untreated genetic conditions blame their parents?
Assume that in the future we would have the option of conducting preventative procedures on human genomes based on predictive genetic diagnostics. Then the question arises as to whether parents would feel pressured to ‘treat’ their unborn children before they are born, so that they live up to the existing norms and standards for ‘normal functioning’ in a scientifically ‘enlightened’ society.
Will we have the courage to bring children into the world if they are considered to be less than perfect?
Will people still be able to make autonomous decisions based on their own values (such as not wanting to ‘play God’ or not wanting to meddle with nature according to one’s own will)?
Do these people risk being excluded from certain social benefits in the form of financial aid or expert advice, if they do not accept offers of treatment?
Might disabled children start blaming their parents, and hold them responsible for missed care during the formative years of their development, if such editing opportunities were in fact publicly funded and considered a ‘reasonable’ option?
Will they hold their parents responsible for a loss of educational opportunities, poor job prospects, or an inability to attract a partner or obtain insurance later in life?
Read More: Will we ever be able to grow organs in a Petri dish?
Economic pressure to ‘opt out’ of bad genes
For those people at high risk of developing genetic conditions later in life, there could come a time in the not so distant future, when they would feel pressured to undertake a number of preventative measures for their own health, in order to live longer, better, and a more independent life in their own home.
Future genetic modification could open up possibilities to carry out preventative procedures before the body has even begun to exhibit symptoms of a given disease.
Such a future scenario was posed by the American scientist, Daisy Robinton from Harvard University at the HealthTech conference on genome editing and other techniques, in Aarhus, 2016.
Together with expected cuts to the public sector and demographic shift to an ageing population with a smaller proportion of people in work, it is not impossible that many will experience a larger economic pressure to limit early or late onset of genetic conditions.
Read More: Scientists find gene switch for “bad” fat
What type of society do we want to live in?
On a societal level, we already see a tendency towards a greater duty of responsibility bestowed upon the individual to care for his or her own health.
Some critics worry about a possible future scenario, where the sick and the vulnerable are no longer guaranteed a minimum degree of medical and societal care and support from the state – and where only the genetically ‘fittest’ have a chance of ‘survival’ in our market-driven society.
This is why we need to have the discussion now to decide what type of society we want for ourselves and for our children. In doing so, we need to reflect on how new technological opportunities will interact with various life choices, cultural values, and economic incentives, if we are to steer these developments in the direction of our choosing.
---------------
Read this article in Danish on ForskerZonen, part of Videnskab.dk.
Translated by: Catherine Jex
Scientific links
- 'A prudent path forward for genomic engineering and germline gene modification', Science (2015), doi: 10.1126/science.aab1028
- 'Human Genome Editing: Science, Ethics, and Governance'
- 'Genome editing reveals a role for OCT4 in human embryogenesis', Nature (2017), doi: 10.1038/nature24033
- Genome editing – an ethical review
- Etisk Råds udtalelse om genetisk modifikation af kommende mennesker (In Danish only)






