Scientists close to a cure for sickle cell anaemia
A new cure for sickle cell anaemia could be on the way following a breakthrough in CRISPR technology
Sickle cell anaemia is an ancient disease and scientists have long known that it is caused by a single variant on one specific gene.
Tens of thousands of people still die of the disease, primarily people of African origin, who suffer from anaemia, fatigue, pain, and premature death.
But this could all change with a revolutionary new technology called CRISPR-Cas9, which could lead to a new gene-therapy treatment that corrects the gene in patients affected by the disease.
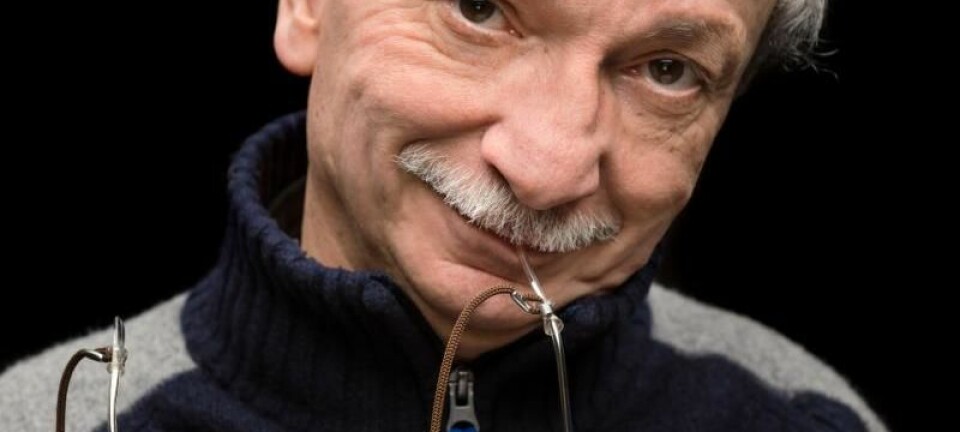
“It’s been fantastic to follow the research project from its inception to the point where it’s basically ready for human trials,” says Dr Rasmus Bak from the Stanford University School of Medicine in California, USA.
The results are published in two studies, one in Nature and one in the journal Science Translational Medicine.
Study provides new framework
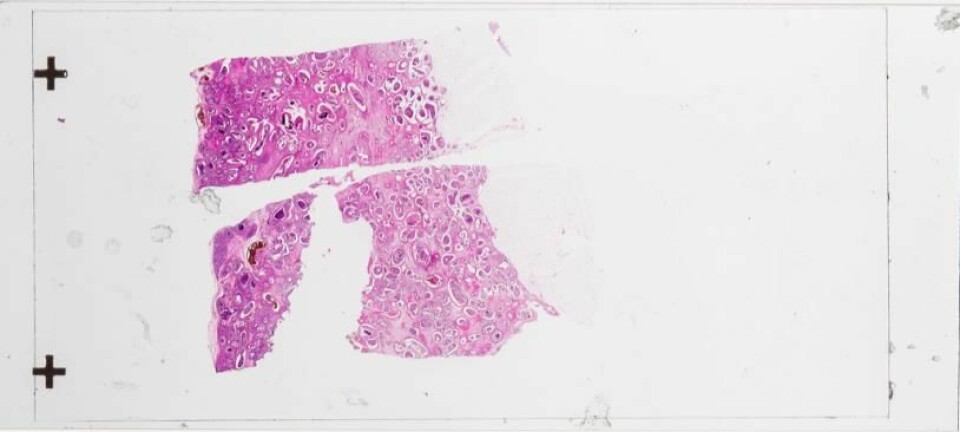
Bak and his team used blood stem cells from patients and corrected the affected gene before injecting them back into the patient.
Scientists have been working on this process for some time, but Bak and his team developed a particularly innovative, new method.
“The study lays a new framework for how we can introduce CRISPR-based changes and how the technology can be transferred to up and coming treatments,” says Professor Jacob Giehm Mikkelsen, who studies gene-therapy at the Institute of Biomedicine, Aarhus University, Denmark.
“This strategy has reached a level where it can be studied in clinical trials of patients with sickle cell anaemia,” says Mikkelsen, who was not involved in the new study.
Cas9 is a molecular pair of scissors
Bak and his team had previously demonstrated that CRISPR technology could be made more effective by modifying the CRISPR-Cas9 chemical system.
The modifications stabilised the molecules so that they survived long enough to carry out the necessary corrections.
Cas9 is a type of molecular scissors that is guided by another molecule and precisely trims the DNA at a set location.
The guide molecule consists of a fragile piece of RNA, which Baks has stabilised.
Helped by a virus
Scientists have now developed a new DNA template that cells use to repair the clipped DNA.
The template consists of the ‘healthy’ DNA sequence, which the cells then copy and thereby remove the mutation in the repair process.
Bak and his colleagues enlisted the help of a harmless virus based on AAV6 (adeno-associated virus serotype 6), which has been used before in clinical trials, to transport the DNA template into the cell.
Bak suggests that the virus-method could be used against other diseases such as β-thalassemia, which is also caused by a genetic mutation in the HHB-gene.
Collectively, the results are so good that we believe we’re ready to initiate clinical trials in humans,” says Bak.
“We hope that the first human trials can begin in early 2018, and then the whole process from inception to clinical trials will have taken around three years, which is extremely fast. It shows what a powerful tool CRISPR-Cas9 is,” he says.
--------------
Read the Danish version on Videnskab.dk
Translated by: Catherine Jex
Scientific links
- "CRISPR/Cas9 β-globin gene targeting in human haematopoietic stem cells", Nature (2016)
- "Selection-free genome editing of the sickle mutation in human adult hematopoietic stem/progenitor cells", Science (2016)