Will we ever be able to grow organs in a Petri dish?
Stem cells can already be employed to replicate any cell in the body and may one day be used to grow entire organs or cure diseases such as Parkinson’s and diabetes. But there are still a number of unanswered questions before the stem cell revolution really takes off.
The human body is composed of many different cell types that enable our organs to perform diverse functions from the production of digestive enzymes and hormones to the generation of sensation and thought.
Stem cells are cells that can both generate a range of these specialised cells and continually produce copies of themselves in a process known as self-renewal.
Given their potential to produce this diversity of cell types there has been an ever expanding expectation of what these cells can do.
Stem cells have been presented as a therapeutic panacea, used as a means to encourage dangerous medical tourism or to sell beauty creams, and touted as an animal free source of meat.
But what are stem cells and what can really be achieved with them?
Read More: ScienceNordic teams up with Science and Cocktails
Many different types of stem cells
To answer this question biologists have studied what these cells can do in the body and what makes them special.
They have found ways to mark them, to purify them, to cultivate them in vitro, and to follow their development to see what they grow into. Stem cells that are able to form any cell in the body are said to be pluripotent and are best exemplified by embryonic stem cells that are derived from human embryos.
While they can be grown indefinitely in a dish in the laboratory, there are also stem cells that remain in many of our organs all our life. For example stem cells in the bone marrow, which multiply continuously to renew the different cells of our blood.
There are also stem cells in the deep layers of our skin that replace the many cells which are shed every day into house dust.
Even though stem cells have very special properties, pluripotent stem cells can also be derived from virtually all adult cells through the process of reprogramming, the subject of the 2012 Nobel Prize in Physiology and Medicine.
Read More: New blood vessels in just seven days
Watch the entire event in the video above (Video: Science & Cocktails)
How do stem cells read their own instructions?
Based on the natural capacity of stem cells to make and regenerate organs, it is natural to think that they could be used to repair our failing body parts.
Although stem cells have the capacity to divide and give rise to daughter cells with specialised function, such as neurons and muscles, they still need to know when and how to do so.
To make this decision they interpret signals from their environment, which instructs every step of their specialisation. It is these signals that scientists have been busy trying to identify.
Every cell in our body contains the instructions to become every other cell in our genes. Embryonic stem cells have the capacity to access all this information, but specialised stem cells have access to a more limited set of instructions, which allows them to only make identical cells. This is to avoid problems such as cancer.
So how does a stem cell access this information, interpret it, and ensure that it is reading the correct set of instructions in the correct order?
Pluripotent stem cells, when left on their own, do it with some randomness, forming balls of cells called embryoid bodies. However, this is an imperfect structure that lacks the correct organization.
Many years of research has been invested into understanding how they can be guided to form specific therapeutic cell types or to organise themselves more coherently into actual organs that could be used for drug discovery and modern medicine.
A large part of this work has involved understanding how cells diversify during embryonic development and what signals trigger them to proceed with the next step in their instructions, and understanding how do different cells interact and instruct each other? This has been a major focus of research during the last twenty years.
Read More: Stem cells strengthen the heart
Stem cell transplantations help third degree burns
Scientists were initially better able to guide the cells residing in adult organs. For example, the stem cells of the blood that reside in bone marrow have been used in clinics since the 1970s.
They can be extracted from a donor and transfused later to the same person or to another compatible patient who has compatible genes.
The cells are transfused to the blood and find their home to the bone marrow on their own. Once they find their niche, they multiply and reform all the blood cells of the patient.
Similar stem cell transplantation has been used to treat third degree burns.
In this procedure, a small piece of skin containing stem cells is removed from a healthy area and scientists can coax the cells to expand or self-renew in the laboratory and generate layers of more mature skin cells to apply to the burn area.
Just this year, similar approaches have been introduced in Europe, using corneal stem cells to generate material to treat the damaged cornea of the eye.
Read More: Scientists close to a cure for sickle cell anaemia
Loss of sight stabilised with stem cell treatment
For many organs we have not yet identified the necessary stem cells, and therefore we have to make these cells using the more complicated task of entraining pluripotent stem cells.
This involves guiding them through the necessary steps to develop into complete organs by mimicking signals they would normally experience during embryonic development and organ formation.
For some organs the cells produced in vitro have reached a sufficient quality to allow human clinical trials.
An exciting example of this was published recently in the New England Journal of Medicine by a team led by Dr. Masayo Takahashi for the treatment of macular degeneration--a disease that causes a progressive loss of sight.
This carefully executed study has enabled the production of retinal pigment cells from human pluripotent stem cells and stabilisation of the disease in the first transplanted patient. This is in stark contrast to a report in the same journal describing vision loss in three patients with the same disease, who had received so called “adipose-stem cells,” in a clinic in Florida associated with a private company now called US Stem cell.
There are both exciting developments coming out of basic research and careful clinical studies alongside dangerous and deceptive promises of ‘stem cell cures’ indicating that new approaches to regulation and patient awareness will be essential as more stem cell technologies move toward the clinic.
Several clinical trials are ongoing for the treatment of Diabetes, Parkinson’s disease, spinal cord injury, and heart failure, among other degenerative diseases.
Read More: Using cells from the mouth to cure blindness
Next revolution: In vitro organs
Although stem cell-based transplantation has taken centre stage for many years, another revolution is taking place that is likely to impact medicinal drug development.
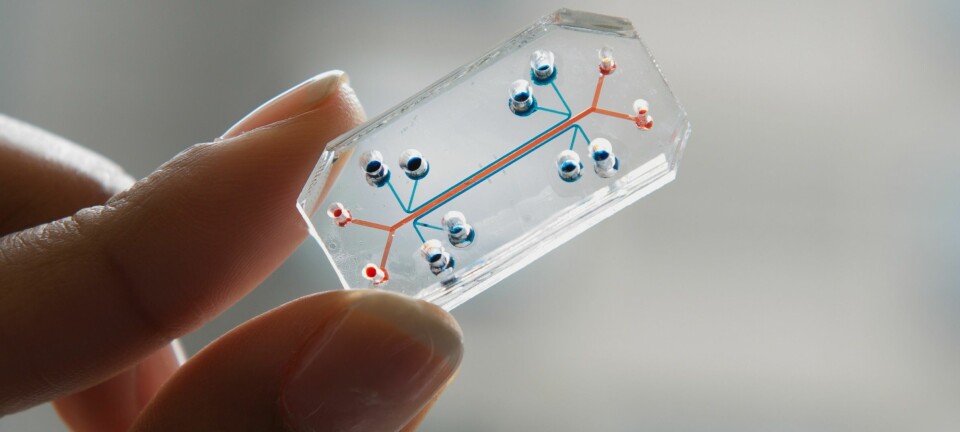
The natural property of stem cells to multiply and generate organs can be exploited not only to make cells for transplantation but also to generate miniature versions of organs in vitro, so-called organoids.
Culture conditions have been developed to seed stem cells in vitro in three-dimensional cultures where they self-organise in space and specialise to form a miniature organ.
Just as embryoid bodies are an imperfect recapitulation of embryogenesis, these structures have many elements of the future organ, but are not perfect. And while these organ avatars are lacking features such as blood vessels, they have been used in specific cases to develop personalised medicine. For example, Hubrecht organoid Technology, a Dutch not-for-profit has been working with insurance companies to use an organoid-based assay, requiring a simple rectal biopsy to test the efficacy of expensive drugs on patients with different genetic forms of cystic fibrosis.
Read More: New material can restore the body's damaged tissue
Immense future potential
The remarkable properties of stem cells to organise themselves into structures even approximating an embryo or an organ is edging closer to becoming a reality.
Understanding how cells interpret instructions, when they access these instructions, and how they talk to each other, has led scientists to think that cells can actually be “taught” to rediscover stem cell programs and be transformed into stem cells.
Providing a cell with the right information means that they can now be induced to take on a new stem cell role, renewing organs, and replacing defective cell types.
But there are still many questions to answer. For example, how is this transformation triggered? How do stem cells interact with each other and other cells to maintain equilibria? And how do cells find new equilibria when their instructional genetic material is distorted by cancer?
Understanding the answers to these questions will lead to new approaches to degenerative diseases and new therapies for cancer. Today, stem cells can be organised into approximations of real organs that can be used to test medicines. But they are still small, imperfectly structured, and lack essential components such as circulating blood. So right now, transplantation should not be considered before these issues are overcome.