Researchers' Zone:

Introducing the poison that inspired Van Gogh and almost killed James Bond: Digoxin
The otherwise innocent-looking flower Digitalis contains the poison that can make your heart stop. That unfortunate effect is also the reason why the poison has been used for treating heart ailments for more than 200 years.
After only a few sips of an otherwise innocent-looking martini, James Bond is shakingly leaving the game of poker against the villain Le Chiffre. The rhythm of his heart is being disturbed by the poison in his veins, causing him to promptly contact the MI6 headquarters. They immediately conclude that 007 is suffering from ventricular tachycardia (VT), a specific type of abnormal heart rhythm, caused by the plant toxin digoxin.
Bond nearly dies but is saved by shock from a defibrillator at the very last moment.
This famous depiction of digoxin poisoning comes from the James Bond movie “Casino Royale”. This toxin is derived from an otherwise harmless looking plant with bell shaped flowers of varying colours such as purple, white, and yellow. The plant is called foxglove (genus Digitalis) and throughout time it has caused many deaths while at the same time saving many lives – both thanks to its potent poison.
The deadly effects of digoxin have been known for over 400 years, and yet even the great 007 almost fell to the poison of a simple foxglove plant- already enough of a reason to explore what makes digoxin so lethal.
The sly features of digoxin
What makes digoxin lethal is also what makes it intriguing, resulting in its frequent appearances in fiction. The fascination for this toxin might stem from some of its many sly features:
- Foxglove is easily accessible due to its wide distribution throughout most of Europe, the US, and Canada.
- Digoxin poisoning is very slow-acting as the toxic effects manifest 30 minutes to 2 hours after ingestion. Also, symptoms of digoxin poisoning can be easily mistaken for other illnesses, both of which makes identification of poisoning by foxglove difficult.
- Lastly, the poisoning will result in heart-attack and ultimately death. However, since heart-attack can be caused by many factors, foul play is often not suspected in cases of poisoning.
Overall, digoxin is easily accessible, difficult to trace, and extremely lethal, which has made the toxin particularly popular as a murder weapon in fiction- and sometimes even in reality.
Admittedly, not many homicides by digoxin have been reported to date, though it is possible that several cases might have been missed due to the exceptionally concealed mechanism of the toxin.
Nevertheless, a few high-profile cases have been confirmed over the years, including one from Toronto's Hospital in 1980–1981. In this case, a nurse was charged with the murder of four babies by poisoning with digoxin. An older case from 1935 in Belgium reports a total of 26 murders via digoxin poisoning by a woman tending to elderly patients.
But how exactly does the poison work?

The heart-stopping mechanism of digoxin
Irregular heart rhythm and eventually heart-attack is what makes digoxin poisoning so dangerous. When digoxin enters the body, it binds a transport protein called the sodium-potassium pump situated on heart cells. Binding of digoxin blocks the pump, ultimately resulting in heart muscle contraction caused by a complex chain of responses.
To understand this mechanism, it is essential to know how muscle contraction works. An important factor for muscle contraction is calcium – high concentrations of it induce contraction of muscle fibres, whereas low concentrations cause relaxation.
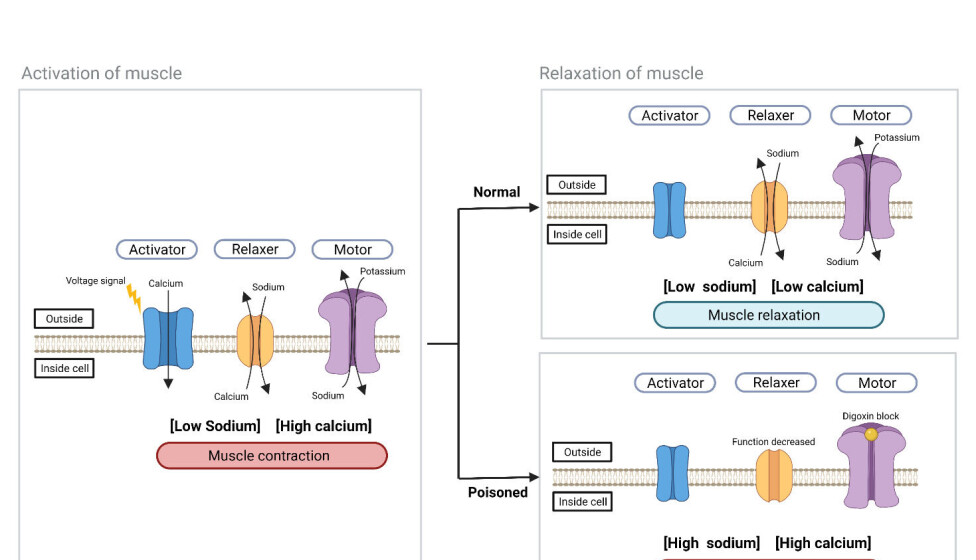
To keep things simple, we can say that this mechanism is primarily regulated by three proteins: The calcium channel (here called the ‘activator’), the sodium-calcium exchanger (which functions as the ‘relaxer’) and the sodium-potassium pump (interpreted as the ‘motor’).
When the activator opens, calcium is imported into the muscle cell, activating the muscle, and causing it to contract. For the muscle to relax, calcium must then be removed by the relaxer.
This transport can only occur if the concentration of sodium inside the cell is low. This is the function of the motor, which keeps sodium levels low in the cell. Thus, one can think of the motor as a battery powering up the relaxer.
When digoxin is present, it blocks the function of the motor, leading to decreased functionality of the relaxer in turn. This blockage causes irregular heartbeats and – in the worst cases – heart-attack since the muscle can’t relax properly.
The dysfunction of the heart rhythm can also lead to symptoms of weakness, disorientation, and even vision disturbances. Interestingly, one of the more commonly observed effects of digoxin on vision is the appearance of a yellow tinge in all objects (See textbox below).
If poisoned, don’t do as James Bond
So how can you counter the effects of digoxin poisoning?
First of all, it is of crucial importance that the functional heart rhythm is regained. In Casino Royale, Bond saves himself with a defibrillator.
In reality, this is not recommended since this method is generally ineffective for correction of heart rhythm in patients with digoxin poisoning.
Instead, the first measure to be considered is the decontamination of the poisoned individual if the poisoning is caused by ingestion.
This should be done by ingestion of activated charcoal since this can bind remaining toxin in the stomach. After decontamination, a digoxin antidote ought to be administered.
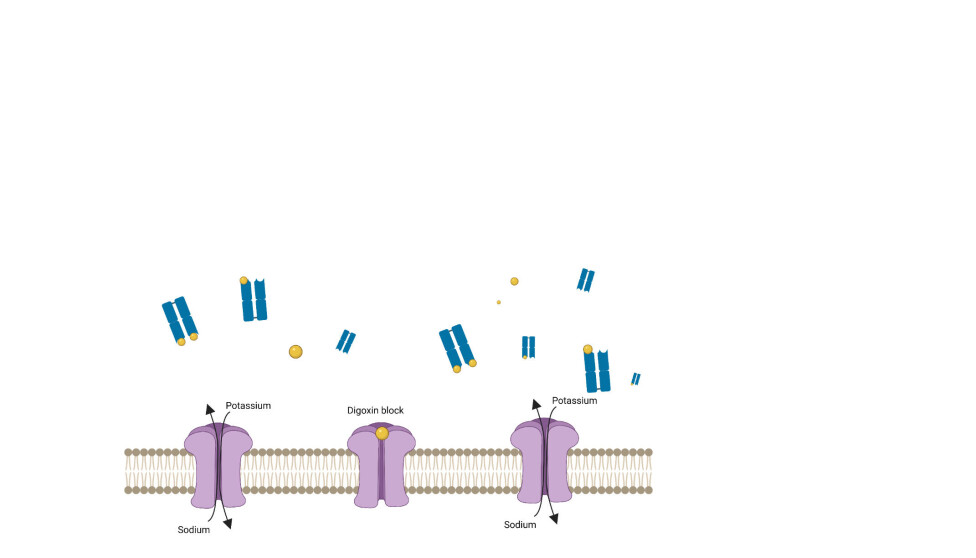
Currently, the only available antidote is called DigiFab. It consists of antibody fragments sourced from sheep immunized with digoxin. When administered, the antibody fragments will bind digoxin, which in turn cannot bind to, and block, the motor.
Treating digoxin poisoning can in general be quite challenging since the toxin is extremely small and therefore spreads widely throughout the body, which makes clearance especially tricky. Having said that, Digifab is still life-saving in the majority of digoxin poisoning cases.
However, the antidote is often not administered due to cost considerations. In fact, the price of this product is very high (up to USD 60k per treatment) which leads to only 25% of poisoned patients actually receiving the drug.
Thus, digoxin poisoning can be a very dangerous situation to be in, without many treatment options.
One of the oldest medicaments for troubled hearts
Despite its lethality, digoxin can also be beneficial to human health when administered at the correct dosage.
In fact, this toxin has been used therapeutically for around 200 years for treatment of heart disease, which makes it one of the oldest medicaments in cardiology.
Digoxin is beneficial in heart disease treatment since it increases the force of heart contractions and reduces the heart rate by blocking the motor.
This action is useful in treatment of several heart conditions such as congestive heart failure (-meaning that the heart does not pump blood efficiently), atrial fibrillation (irregular and excessively rapid heartbeat) and other heart rhythm conditions.

Due to the high prevalence of heart disease in the 21st century and the low price of 0.47 – 0.56 USD per pill, digoxin is widely used globally - around 66,000 patients in Denmark receive it each year and it was the 184th most prescribed medication in the United States in 2018, with more than 4 million prescriptions. Unsurprisingly, most of the patients receiving the drug are elderly, with nearly one-third being 85 years of age or older.
Thin line between treatment and poisoning
Although many patients are treated with digoxin, it carries serious risks if administered incorrectly.
In fact, the toxic dose of digoxin is only 1.6 times that of the therapeutic dose, meaning that minimal overdosing can result in severe poisoning.
Dosing of digoxin is not an easy task since differences in body size, age, and multiple other factors can change the response of different patients to the therapy.
As a result, toxicity often occurs among chronic users (especially in elderly patients or patients with renal impairment) , with a mortality rate between 7-30%.
Additionally, it is estimated that over 5000 emergency department visits for digoxin toxicity occur annually in the United States. Thus, poisoning from clinical use is actually the most common reason for digoxin poisoning-not malicious assassination attempts like the one depicted in Casino Royale.
Because of this, other drugs are now preferred for treatment of heart disease, such as Angiotensin-Converting Enzyme (ACE), Angiotensin Receptor Blockers (ARBs) and Beta-blockers.
In general, the matter is still debated and differences in heart conditions and patient response to different drugs all affect which drug option is the best in each individual case.
Thus, there is a need for either safer dosing or improved options for treatment of toxicity. Otherwise, digoxin is likely to be replaced by alternate drugs in future heart disease treatment. In the meantime, we can at least take a valuable lesson from 007’s life-threatening encounter with digoxin: no matter how fancy the event, never accept a martini from a mysterious stranger.
The article was originally published on our danish sister site Forskerzonen.
References
‘Emergency Department Visits and Hospitalizations for Digoxin Toxicity’, Circulation: Heart Failure (2014), DOI: 10.1161/CIRCHEARTFAILURE.113.000784




