Can vitamin D help against COPD?
Chronic obstructive pulmonary disease (COPD) patients with deficient levels of vitamin D displayed poorer lung functionality and more rapid deterioration of lung function in a three-year period, according to new research.
Chronic obstructive pulmonary disease (COPD) is an inflammatory lung malady that permanently reduces lung capacity. Some COPD patients get by for a long time while others suffer a steeper and quicker slide into inadequate lung functionality.
What causes the difference? Louise Jeanette Pauline Persson, who works with respiratory diseases at Haukeland University Hospital, sought an answer. Persson found out that patients with serious COPD also had low levels of vitamin D.
Creates its own antibiotics
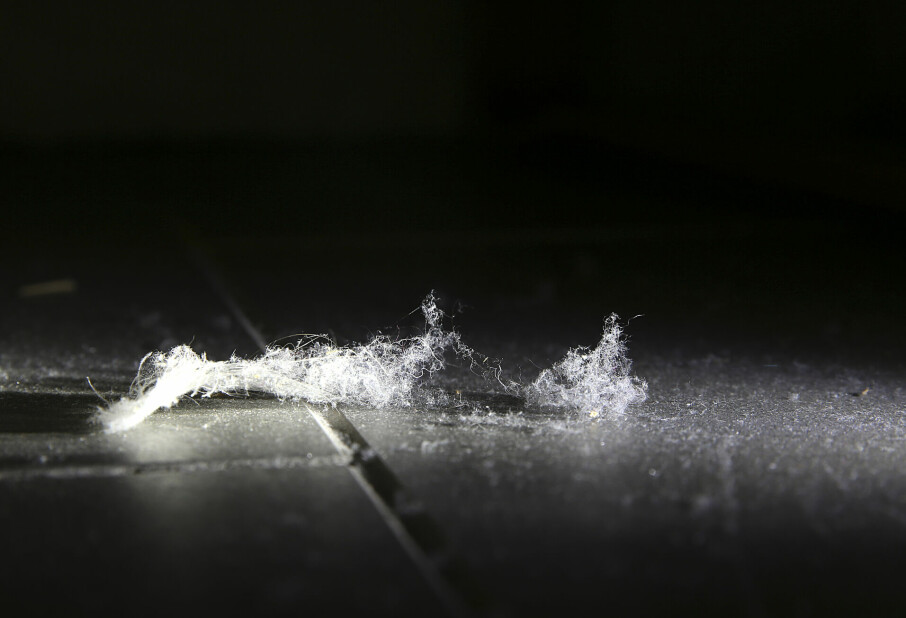
Some COPD patients are more prone to contracting lung infections which exacerbate their condition and the disease runs a faster course.
The mechanisms behind this have not been fully understood. However, newer research points to interplay between the immune defence system and bacteria or viruses in the lungs. The degree of infection has an impact on the general development and outcome of the disease in COPD patients.
Antibiotics created by the body itself might affect this interplay and bolster the immune defence system against respiratory infections. These antibiotics are called antimicrobial peptides.
Evidence has surfaced recently showing that vitamin D can impact the immune defence and inflammation processes in a positive way.
Examined 750 persons
Persson compared vitamin D levels amongst 433 COPD patients against 325 healthy persons who comprised the control group. Many in both groups had vitamin deficiencies but the frequency of lower vitamin D levels was greater among the COPD patients.
The COPD patients with low levels of vitamin D had poorer lung functionality than those with higher levels of the vitamin at the time the study started.
Their lung functionality also went downhill more quickly in the course of a three-year period, even if they did not suffer more frequent respiratory infections.
The difference in vitamin D levels between the COPD patients and the control group was especially large in the fall and summer.
Several of COPD patients with low vitamin D levels were either overweight or underweight, depressed or used steroids medicinally.
Doubts about supplements
Would this mean that it would be smart for COPD patients to take vitamin D supplements?
“Such supplements are not recommended in treatment to curb COPD development because current research has not shown a beneficial effect of vitamin D supplements for lung function, infections or lung inflammation,” explains Persson.
However, she adds that vitamin D has documented effects against osteoporosis. So if a COPD also has this brittleness of the bones, taking supplemental doses of the vitamin would probably be advised.
Check more frequently
In general, the elderly and those who spend little time outdoors run a risk of insufficient vitamin D.
“Our data indicates that this is also an issue among Norwegian COPD patients. So they should check their vitamin D levels more often and take supplements if they are below the recommended level.” says Persson.
A recent OECD report places Norway with one of Europe’s highest mortality rates from COPD and other lung diseases.
Overactive immune defence?
Persson also compared the levels of two types of antibiotics produced within the bodies of patients. These assist in our natural immune defence systems and one of their functions is to fight inflammations.
The COPD patients had other levels of these two substances in their lungs than did persons in the control group. Such levels also varied with the degree of infection in the lungs and the presence of respiratory infections.
“The COPD patients in a stable phase of the disease had higher levels of these peptides than those in the control group. These conceivably strengthen the immune defence of the patients. Contrarily, they had stronger inflammation processes in their lungs, linking to an immune defence that overshoots the target without protecting better against infection,” says Persson.
Amongst the patients with acute complications the levels of these peptides differed even more from those amongst the stable COPD patients. Patients with very high levels of one of the peptides ran higher risks of a later aggravation of their disease.
The finding shows that antimicrobial peptides could have an impact on the progression of disease and COPD infections.
“This bolsters the theory that the progression of COPD links to an activated immune defence involving immune cells and inflammation processes.”
She adds that other research has also indicated that COPD partly has an autoimmune component.
Translated by: Glenn Ostling
Scientific links
- Louise Jeanette Pauline Persson: Vitamin D and antimicrobial peptides in COPD Results from the Bergen COPD Cohort Study. Doctoral Dissertation, University of Bergen, 25.11.2016.
- L. Persson et al.: Chronic obstructive pulmonary disease is associated with low levels of vitamin D. Abstract. PLoS One. 21 June 2012. doi:10.1371/journal.pone.0038934
- L. Persson et al.: Vitamin D, vitamin D binding protein, and longitudinal outcomes in COPD. PLoS One. 24 March 2015. 10(3)