Norway has secured access to a COVID-19 vaccine. So what is it actually made of?
And what will it take for the vaccine from Oxford University and AstraZeneca to succeed?
Norway will have access to the so-called Oxford vaccine against COVID-19 through its agreement with the EU. If the vaccine is approved, that is.
So what will it take for it to work effectively? And what could cause it to fail?
To answer these questions, we need to understand what the vaccine actually is. It’s not made in the classic way – where the vaccine contains damaged pieces of the virus you’re vaccinating against.
This vaccine does not contain the coronavirus at all.
«DNA is used in the vaccine,» says Tor Kristian Andersen. He is researching vaccines at Oslo University Hospital.
The DNA does not originate from the virus itself but is genetically engineered.
It contains the recipe for the 'spike protein' of the coronavirus. You know, the feature that gives the virus its distinctive appearance.
Has to get into the cells

But this vaccine, which was developed at Oxford University in collaboration with the pharmaceutical company AstraZeneca, contains more than just DNA code.
In fact, it contains a completely different virus than the coronavirus.
Specifically, it contains a cold virus called adenovirus that is manipulated so that it can’t replicate, Andersen explains.
«The vaccine only uses the virus as a delivery method for the DNA that encodes the spike protein,» says the vaccine researcher.
In other words, the researchers have used genetic manipulation to replace some of the normal genes for the common cold virus with the spiked protein gene of the coronavirus.
Even though the virus can no longer replicate, it can enter our cells.
«The vaccine depends on getting into the cells and into the cell nucleus. And the nice thing about viruses is that they have mechanisms to do just that,» says Andersen.
So when the vaccine is injected into a muscle, it initially ends up between the muscle cells. However, with the help of the genetically modified virus, the spike DNA enters some of the muscle cells.
And there our cell’s protein-making equipment is ready to read the 'recipe' for the corona gene.
Cold virus from chimpanzees
An interesting detail about the cold virus in the vaccine is that it doesn’t originate from humans.
It originates from chimpanzees.
«There’s a pretty good reason for that,» says Andersen.
Using a human virus is a bad idea. If you’ve already caught a cold with a virus similar to what you get in a vaccine, your immune system will attack the vaccine virus.
«This means that when the vaccine is injected into the body, it has almost no time to do its job in the cells before the virus is removed by the person’s immune system. So by using a virus that originates from chimpanzees, humans have no history with that virus,» the researcher says.
Since this chimpanzee virus has been altered so that it cannot make copies of itself, it doesn’t spread in the bodies of people who are vaccinated.
So what does it take for this vaccine to actually protect us from the coronavirus?
Immune system has to remember
If all goes as the researchers are imagining, our muscle cells will read the DNA code, manufacture the coronavirus spike protein and transport the spikes out of the cells.
Then the immune system sounds the alarm that something foreign is in our body, Andersen explains.
Ideally, the immune system should learn what these spikes look like by making antibodies as well as by storing the information in so-called T-cells for later.
This will enable our body to recognize the real coronavirus if we become infected later.
Oxford researchers have tested the vaccine on rhesus monkeys and infected them with the coronavirus. The monkeys that received the vaccine were protected against corona pneumonia, according to a study available in the bioRxiv database that has not yet been peer reviewed.
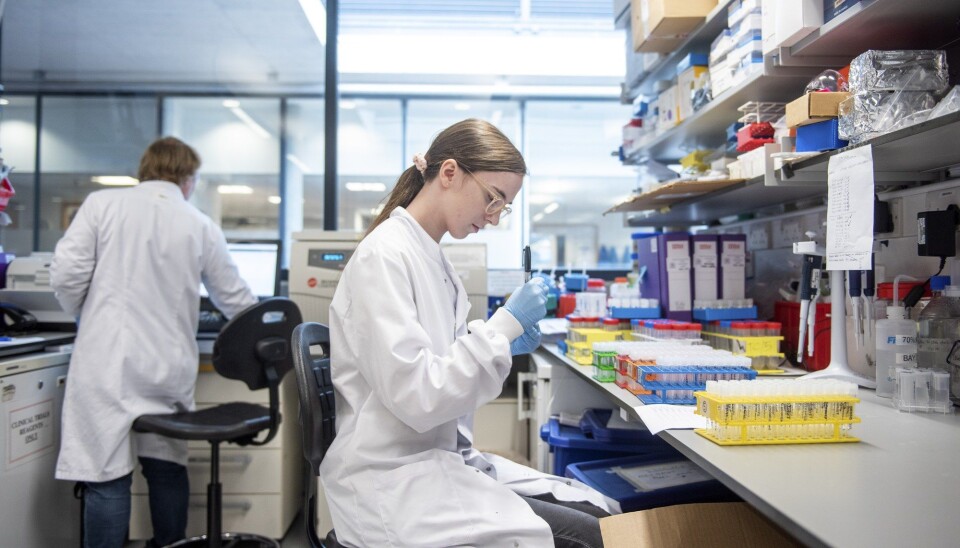
The researchers also tested the vaccine on about 500 people in a combined
phase one and two study published in the The Lancet.
Antibodies found in blood of test subjects
These test subjects were not exposed to the disease itself, as the monkeys were, but the researchers took blood samples from some of the participants. The tests showed that their immune system had responded to the vaccine.
Antibodies to the coronavirus spike protein were found in 90 per cent of those tested. The test subjects had also developed several T-cells that recognized these spikes.
Now the testing is in phase three, which means the vaccine is being tested on several thousand people.
This phase will show if the Oxford vaccine triggers a large enough immune response in the body to actually provide protection against the disease.
The presence of antibodies and T-cells does not mean that vaccinated individuals are guaranteed to become immune to the virus.

Only one part of the virus
Compared to classic inactivated vaccines, the Oxford vaccine activates the immune system more narrowly.
In the genetic vaccine, the immune system is only exposed to the characteristic spike protein.
This is where the classic vaccines may have an advantage.
«The vaccines that are made from inactivated viruses are a bit like hitting the bass drum,» says Stig Tollefsen. He is the Head of Strategic Science at the vaccine coalition CEPI.
If a vaccine contains the coronavirus itself, our immune system can learn to recognize several parts of the virus, thus training a broader repertoire of the immune system in individuals who receive the vaccine, according to Tollefsen.
«At the same time, there are many indications that targeting the vaccine against the spike protein actually generates antibodies that are more than sufficient to protect against disease,» Tollefsen says.
Easy and cheap to produce
The Norwegian-led CEPI, which was founded in 2017, has invested millions of Euros in the development of nine different vaccines so far, which use various vaccine technologies. Seven of them are being tested on humans. One of these is the Oxford vaccine.
Tollefsen won’t rank the vaccines CEPI has invested in. But he says that one of the advantages of the Oxford vaccine is that it's easy and cheap to produce.
«I think genetically modified vaccines are the future of vaccines, at least more than inactivated viruses,» he says.
This applies to genetically engineered vaccines with DNA, RNA or proteins as the active ingredient.
If we understand how the immune system reacts to a disease, genetically modified vaccines can ensure that the right parts of the immune system are trained, Tollefsen explains.
But for the Oxford vaccine to be approved, just the fact that it works is not enough.
It also has to be safe.
Possible side effects
What side effects could people face from the vaccine that Norway has secured through the EU?
The researchers found no serious side effects in first two testing phases on humans. However, some participants in the study reported fevers, chills, muscle aches, headaches and general malaise, according to the Lancet study.
One objection to gene-based vaccines is that they can alter the genetic material in the cells they enter.
Andersen has previously rejected several allegations from a campaign against letting Norwegians be 'test rabbits for GMO vaccines' in a fact check on faktisk.no.
«This issue has been investigated through several independent clinical studies where the results show that DNA vaccines have an impeccable safety profile, without signs that vaccinated genetic material can be affected by the vaccine,» the researcher says.
Andersen also reminds us that just living a normal life – exposure to sunlight, the food we eat, and the infections we get – constantly disrupts our DNA.
«The studies that researchers have done involving DNA vaccines show that they affect the genetic material 1000 times less than just living. So the risk is very low,» says Andersen.
Translated by: Nancy Bazilchuk
———
Read the Norwegian version of this story on forskning.no