This article was produced and financed by Norwegian centre for E-health research - read more

A shared national patient medication list will soon be tested in Norway
The shared medication list is a new electronic overview that health professionals in Norway will be testing out in 2020. What do the authorities want with the new system? What does research say about the usefulness of such medication lists?
In Norway, many people have great expectations that healthcare workers will be able to use the so-called Patient's Medication List - a shared, national medication list which will give health professionals updated information about patients' medicine use.
Next year, testing of the new system begins and it will be brought into use in 2022.
The shared medication list shall make information about the patient's medicines available to health professionals in a single, national overview. The reason for the introduction is a lack of information flow about patients' drug treatment across the health services, such as general practitioners, hospitals and pharmacies.
General practitioners, emergency services, primary care services and hospitals will all benefit from the solution.
The Norwegian Centre for E-Health Research is performing research on several of the government's new technology solutions, including the Patient’s Medication List. The goal is to obtain as much knowledge as possible - and preferably as early as possible - so that the use of new technology in health services is of good quality.
Collected experience from eight countries
Many countries want to get a shared medication list because medication errors is a serious problem. So far, no one has managed to create a national overview.
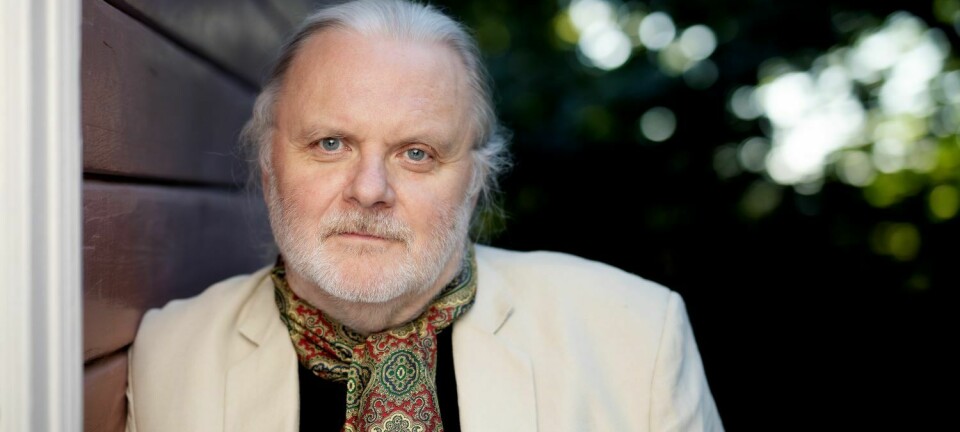
"We have reviewed nine studies from eight countries. All studies are from the primary health service. Then we made a summary from the studies on how health professionals and patients use a shared electronic medication list", says Unn Sollid Manskow at the Norwegian Centre for E-Health Research.

Manskow has looked at the use of electronic medication lists together with her colleagues Karianne Lind and Trine Bergmo. Their literature review can give valuable information on experiences and effects. They studied research articles from Norway, Sweden, the United Kingdom, Germany, Switzerland, Austria, the United States and Canada.
Today, it is a challenge that health professionals do not have access to the same information about patients' medications, since they are stored in different patient records and systems that are not connected. Medication errors threaten patients' health and can cause illness and death.
Manskow and her colleagues studied three areas in their research:
1. Different IT solutions in several countries
2. Patient safety and quality of services
3. The experiences of health professionals and patients
Local and regional solutions
Several of the countries had created IT solutions for sharing medication lists at the local or regional level.
"And then there are plans to create national systems. But no country has done it yet. That is why we found little research, even from countries that we know are planning on doing this, such as Denmark and Finland", says Manskow.
Since there were so few research articles, she made direct contact with people in, among others, Denmark, who were involved in national IT projects in the health services.
"In Denmark they are working to implement national solutions but they are not there yet", informs Manskow.
Easy to use, good training
Manskow and her coworkers found useful insights in their review about patient safety and quality of service.
"A study in the UK found that a shared medication list led to less risk for patients. Health professionals had fewer errors in medication lists and more faith that errors and injuries could be prevented", she says.
A study from Austria pointed out what is important for doctors and pharmacists: A medication list had to be national and everyone had to use it, the interface had to be simple and the users – the health workers – had to receive good training.
"After looking at research results from Germany, Switzerland and Austria, we saw that everyone wanted to improve the safety of medicines management. But things have gone slower than expected and none of them have managed to create national solutions".
Manskow noticed that these three countries had different strategies for health professionals.
"It was not obligatory for all employees to use the medication list. In Switzerland it was voluntary, while they were required to use the list in Germany and Austria. This is interesting and something we take with us", she says.
In a Swedish study from 2014, researchers investigated the experiences doctors had when the Swedes went from local to regional drug lists. The doctors thought it was positive that they got a more complete list and access to information. However, there were downsides too.
"In the list they discovered prescriptions that were no longer relevant to the patient. They also couldn't share the list between regions. An important, overall question emerged: Who had the main responsibility for the list, was it the GP or the specialist in the hospital? In Norway, we are used to thinking that it is the GP who knows the patient best", Manskow points out.
Nothing about people's health
The e-health researchers also wanted to look at the patients' health. And that's when they discovered something central:
"None of the research we read said anything about whether people had fewer injuries or better health because the health workers had new IT systems. More research is needed", Manskow emphasizes.
"We need to find out how new computer systems affect the health of patients. There are great expectations that new solutions will lead to fewer deaths, hospital admissions and fewer injuries."
The patients were cautious optimists
Patients had mixed experiences after trying out solutions with shared medication lists.
"In a study from the UK, patients said they were more confident in their own medication management, that they communicated better with health professionals and became more involved", says Manskow.
"In another study from the same country, they had looked at the summary care record, which has important information that health professionals can see, regardless of the place of treatment. They found that few knew about it, and that almost no one used it or knew how to log on. Some residents said they did not want their data stored there. But of course a lot can be behind this, not least the lack of information about what this is and what the data will be used for".
Many thought it was important and good that people could become more involved in their health by accessing their own information.
"In summary, I would say that we found few studies and with varied experiences. The actors had different views of how IT solutions worked. The countries have created different solutions, but so far, no one has created a national medication list."
One thing in particular got Unn Sollid Manskow’s attention:
"Very few researchers had asked the nurses about their experience with medication lists. They had almost only interviewed doctors and pharmacists. The reason is probably that the latter two are essential in prescribing and giving out medicines. But it is often nurses who order, distribute and observe the effects of medication. The danger of wrong medicine use is great in every part of the chain, and we also need to know what the nurses' experiences are", she concludes.
Reference:
U.S. Manskow, K.F. Lind, T.S. Bergmo: Digital solutions for a shared medication list. A narrative literature review. SHI 2019: Proceedings of the 17th Scandinavian Conference on Health Informatics. Oslo, 12-13 Nov. 2019. Linköping University Electronic Press, p. 7-12.
———
Read the Norwegian version of this article on forskning.no