Why do schizophrenia patients die earlier than other people?
The average life expectancy of Norwegians with schizophrenic disorders is 62 years. If you also have a drug problem, it goes down to 47 years. “It’s difficult to understand why this isn’t prioritized by the health services,” says a veteran psychiatric researcher.
“The disease costs more than all cancers. More than all heart disease. More than all rheumatic disorders.”
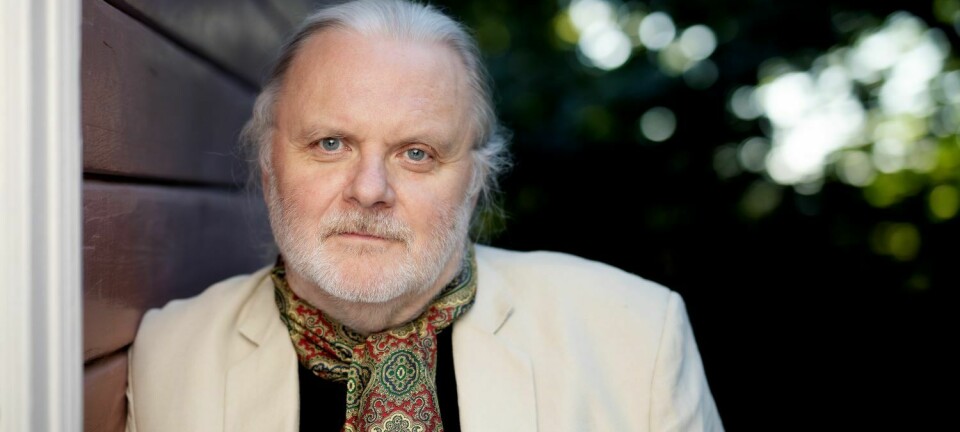
Ulrik Fredrik Malt finds it a paradox that we’re not spending way more money on schizophrenia, given how great the costs are.
“I would guess that a lot of politicians are middle-aged and older. They’re actually more concerned with bodily diseases that affect their own age group. In my view, they don’t care about the most seriously mentally ill among us,” he says.
He recently held a lecture under the auspices of the Norwegian Brain Council and Nansen Neuroscience Network in Oslo, in which he criticized both the health service and politicians for not taking strong enough hold of a problem that costs society so much.
Much more than psychology
Most people know that people with schizophrenic disorders often have hallucinations, delusions, and thought disorders.
Not many people know that these patients also experience changes in hormones and lung function, intestinal disturbances, changes in their immune system, increased risk of autoimmune diseases, changes in temperature regulation, menstrual disorders and altered heart rhythm.
“A lot of people think that schizophrenia is just psychological, and they don’t understand that this is a disease that affects the whole body,” says Malt, who is a professor emeritus in psychiatry.
Anxiety can be harrowing
The costs of schizophrenia are a big burden for society, but it is the patients and their relatives who endure the greatest costs and suffering.
Malt highlights anxiety, which he says is perhaps the worst side of the disease.
“The anxiety can be harrowing. It can feel like losing one’s identity. Disintegrating. One of my patients constantly had to look in her passport to know who she was,” says Malt.
He notes that schizophrenic disorders come in many variants. Some individuals with the disease are high functioning, but the sickest people have a severely impaired ability to function.
And not infrequently, this also leads to substance abuse.
Inequality has increased
A Norwegian study from 2018 with almost 13 000 patients shows that people with schizophrenia or a serious drug addiction have, respectively, four and seven times as high a risk of premature death as other Norwegians.
The risk of suicide and overdose deaths are especially elevated.
And yet this group also suffers many lost years of life from cardiovascular diseases, cancer and respiratory infections, as compared to the population average.
Researchers Ina Heiberg and Anne Høye at UiT Norway's Arctic University told Norway’s independent online health news channel Dagens Medisin that the study shows that the inequality in mortality between people with schizophrenia and the rest of the population has actually increased since the previous national study from the 1970s.
Important to see the whole patient
Nearly half of us will someday have a mental illness. About 30 per cent will struggle with it for a year or more.
Using a narrow definition, around one percent of the population will be affected by schizophrenia. When using a broader definition, it is about two to four percent.
More people suffer from schizophrenia in cities than in rural areas. The disease is also more frequent among immigrants.
Genetics makes these patients particularly vulnerable to developing schizophrenia when they are exposed to stress and pressure, for example when living in close proximity to others or coming to a new country where they don’t know the social codes, Malt says.
However, stress is not the explanation for schizophrenia. This is largely a genetic disease.
Today, observable symptoms and signs typically form the basis for a diagnosis.
Psychologists often make the diagnosis and rely primarily on psychological symptoms. Malt believes that this is problematic.
“The whole patient has to be considered, by both doctors and psychiatrists. Psychologists are important for rehabilitation, but we also need someone who can see the larger picture,” he believes.
Lifestyle also significant
Petter Andreas Ringen, a psychiatry specialist, says the complicated connection between genetics, lifestyle and drug use is the reason that the mortality rate of schizophrenic disorders is so high.
He says that there is a tremendous prevalence of smoking, substance abuse and low physical activity in this patient group. Many patients are also socially isolated, which in itself increases the incidence of poor health and early death.
These lifestyle problems aren’t picked up by the health care system,” Ringen says.
He believes that prevention has to begin early, as soon as the disease emerges.
Fall through the cracks
Part of the problem has been that these patients fall through the cracks in the health service. There is a lack of contact and cooperation, especially between the psychiatry and somatics disciplines. No one has taken on responsibility for coordinating the services.
The national standardized package of procedures for mental health and intoxication introduced by the government starting 1 January 2019 is intended to resolve many of these issues. The package should offer patients more comprehensive and predictable treatment.
The package will also demand greater accountability regarding which examinations the patient should receive and who is responsible for following up. The distance between somatic and mental health will also decrease.
------------------------
Read the Norwegian version of this article at forskning.no