When your immune system becomes your worst enemy
Our innate immune response can sometimes be so drastic that it ends up harming us in its attempt to save us from serious infection.
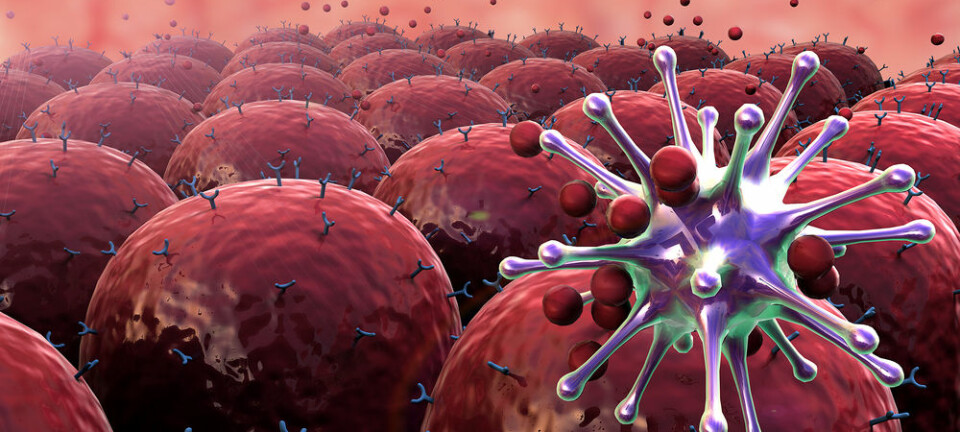
The immune system, which is our best weapon against uninvited guests such as bacteria, is built like a defence against invasion.
Front-line soldiers continuously scout for enemies and sound the alarm when danger is detected. We call this the ‘innate immune system.’
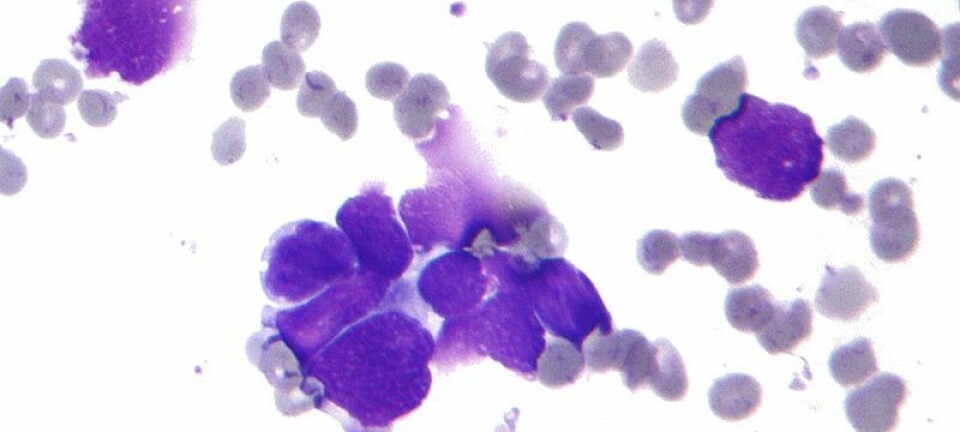
It does not matter if they haven’t seen the enemy before as they simply regard all foreigners as hostiles. The foot soldiers consist of proteins and white blood cells, which react against the enemy—and generally they do their job well.
But the innate immune system can also turn into our own worst enemy, when it becomes overactive or is tricked into attacking the body. This can lead to cardiovascular disease, exacerbate septicaemia (blood poisoning), or neurological diseases, and in the worst case scenario they can cost the patient their life.

Read More: Vitamin D can boost immune system’s fight against one of the world’s biggest killers
Immune system can ‘explode’
There are two problems in particular with the innate immune response.
First, the innate immune system is the first responder to the scene and can become overactive when it meets serious infection, major injuries, or burns.
The intention is to kill the bacteria or repair the damaged tissue, but the result can be an ‘explosion’ that not only fights the invasive microbes but also attacks the host (patient).
This causes an inflammation in the body, which can get out of control and end up doing more damage than the bacteria ever would. In the worst case scenario it can lead to organ failure and death.
All of us have an innate immunity that can ‘explode.’ Think of it as an undetonated bomb, which only causes harm when it actually explodes.
The immune system can react against the body’s own tissue
Luckily, this rarely happens.
Normally, the immune system takes care of the bacteria, but if it spreads to the bloodstream, as is the case in septicaemia, it can sometimes initiate a type of ‘immunological suicide’ where our innate immune system harms us in an attempt to save us.
Second, the innate immune response can react against the body’s own tissue in the event of an injury such as an acute heart attack, rejection of a transplant organ, or a chronic vascular disease that leads to atherosclerosis.
In cases such as these, the foot soldiers do not react against the enemy invaders, but against our own damaged tissue.
The immune system will help to repair the damage, but if it is too extensive the foot soldiers can misunderstand the situation and start a war in an attempt to fight the supposed outsiders.
Read More: Asthma might weaken the body’s immune system
Previous attempts to dampen the immune system failed
When the foot soldiers register a threat, they begin to inform others to react, and an entire battalion of biological actors set to work. These molecules—cytokines—cause inflammation.
Scientists have tried to study a number of them before without success. They tried to inhibit them while treating patients for blood poisoning and a range of other diseases, where the innate immune system can overreact and harm the patient.
All previous clinical trials were halted before the remedy could be used. So what do you do?
Read More: UV-treated milk strengthens premature babies’ immune system
Two central systems must be blocked
One of us, Tom Eirik Mollnes, suggested that the only way you can dampen the explosion of the innate immune system response is to block certain groups of foot soldiers before they can cause inflammation and damage organs.
This treatment targets two particular groups, which react as soon as danger approaches. They are two of the most important systems in the foot soldiers’ war:
- The Complement System
- Toll-like receptors (TLR)
Mollnes and his team discovered that it is significantly more effective to inhibit these systems right from the start, before the explosion in inflammation can happen. We’ve now demonstrated this in samples of human blood in the laboratory.
We then showed that it also worked in both mice and pigs suffering from blood poisoning. They survived longer when the molecules in these two central systems (C5 in the complement system and CD14 in the TLR family) were simultaneously inhibited.
These results were completely at odds with previous studies, which blocked single molecules released after the complement system and TLR were activated.
So we suggest that blocking these two systems immediately when they discover danger is the most effective treatment in cases where a patient is at risk of death by the immune system’s overly explosive counter attack.
Read More: Using our body’s immune system to fight cancer
Foot soldiers misinterpret their duties
There are also a number of cases, which are not nearly as dangerous as blood poisoning, where it may also be relevant to block our immune system response.
This applies when groups of foot soldiers (the complement system and the TLR) misinterpret their duties.
The think they should attack an enemy, but instead attack the patient’s own damaged tissue, which they don’t recognise as a part of the body due to the damage.
This is the case for a number of diseases, such as atherosclerosis, kidney disease (including rejected transplant organs), and autoimmune disease (such as arthritis), where the body produces antibodies against its own tissue and activates the complement system.
The same problem occurs in dangerous neurological diseases and any number of other diseases where it could help to inhibit the complement and/or TLR systems. We therefore need to test medicine that inhibits both systems simultaneously.
We hope that our strategy can form the basis of future treatments for a range of diseases caused by the innate immune system.
---------------
Read this article in Danish at ForskerZonen, part of Videnskab.dk
Translated by: Catherine Jex