Researchers' Zone:

How your immune system combats infections like COVID-19
Your immune cells can be found everywhere in your body and without hesitating they will fight against any intruder to ensure your well-being. But how much do you know about your immune system and the way your immune cells handle infections like COVID-19?
These days, politicians, scientists, and healthcare professionals around the world are working day and night to stop the spread of COVID-19.
Meanwhile your immune system is working maybe even harder to ensure that you will not get critically ill, if you contract SARS-CoV-2 – the virus that causes COVID-19.
But your immune system does so much more!
The primary job of the immune system is to protect you against everything that is not supposed to be in your body. This could be virus, bacteria, or other disease-causing microorganisms. It could also be your own cells if they do not behave as they are supposed to.
For example, your own cells can get infected with virus, they can get too old and dysfunctional, or mutations can occur turning the cells cancerous.
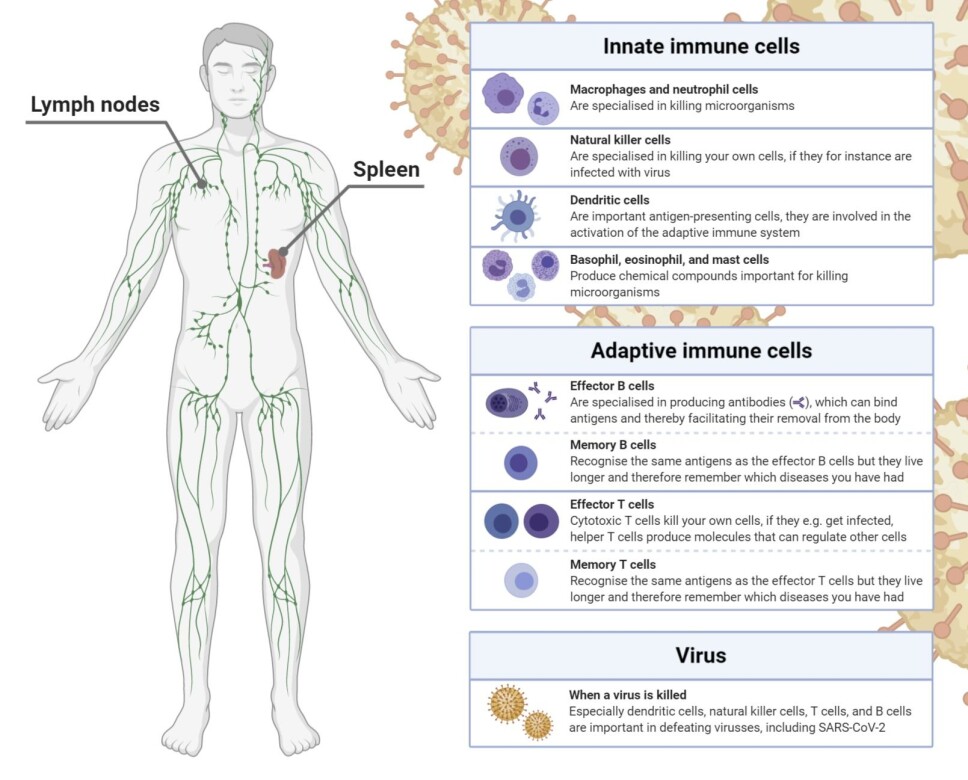
Your immune system can carry out its critical functions because it is a complex machinery composed of various cell types and molecules. Traditionally, it is divided into the innate and adaptive immune system.
So how does it work? How does your immune system combat infections? This article will guide you through the general functions of your fascinating immune system.
The barrier function of your innate immune system
First, it is important to get familiar with the differences between the innate and adaptive immune system.
The innate immune system is effective already from birth. It is made up of physical and chemical barriers along with specialised immune cells.
- The physical barriers comprise all the outer layers of your body. That is, the body parts that are in contact with the outside world (for instance your skin and the surfaces of your gut).
- The chemical barriers consist of protective chemicals in and on your body. These include your saliva, gastric fluids, and tears. These body fluids contain chemicals making it difficult for most microorganisms to survive.
Together, the physical and chemical barriers make it tricky for microorganisms to enter your body.
The innate immune system is the first line of defence against microorganisms, your foot soldiers
If a microorganism manages to break through the barriers, the innate immune cells are activated.
Most microorganisms have certain characteristics, which distinguish them from your own cells. This is similar to the fact that humans have hair, while birds have feathers. The innate immune cells have receptors (sensor molecules) on their surface, which allow them to recognise these general characteristics of most microorganisms.
You can also say that the receptors function as pattern detectors. They are only activated when they detect particular patterns from microorganisms.
When the receptors are activated, a signal will be turned on telling the immune cells that it has encountered a foreign organism. Consequently, the immune cell initiates a response against the intruder.
Most infections are actually defeated by the innate immune response before they make you feel ill. However, in some cases the innate immune system is inadequate. In such situations, the innate immune system alerts the adaptive immune system, so the adaptive immune cells can be activated and recruited hereby providing more specialised help.
The adaptive immune system is your second line of defence, your special forces
Some innate immune cells are specialised in killing microorganisms. Others collect small fragments of the microorganisms, that they present to and thereby activate specialised adaptive immune cells.
These small fragments correspond to the fingerprints of the microorganisms and are termed antigens.
The adaptive immune system consists of T cells and B cells.
T cells and B cells have certain receptors on their surface called T and B cell receptors, respectively. These receptors recognise antigens presented by the innate immune cells.
Every T and B cell has many copies of the same receptor on their surface. Therefore, each cell is specific to one particular antigen.
Your body houses billions of T and B cells with millions of different T and B cell receptors, which makes your adaptive immune system capable of recognising almost every microorganism.
It takes time to activate the adaptive immune system (several days), as only few T and B cells will recognise a specific microorganism. The activation also takes time, as your T and B cells primarily reside in your spleen and lymph nodes when they are inactive.
If you get an infection, like SARS-CoV-2, antigens from SARS-CoV-2 must first be carried to your spleen and lymph nodes. At these locations, the antigens must be recognised by the right T and B cells, allowing your adaptive immune system to become activated.
How the activated adaptive immune system works
After activation, T and B cells divide extensively. In that way more adaptive immune cells able to recognise the invading microorganism are made. These cells will begin combatting the intruder. To do so, the activated T and B cells will either become effector or memory cells.
The primary function of effector B cells is to produce antibodies. Antibodies bind antigens and can therefore bind microorganisms like SARS-CoV-2.
An antibody bound to a microorganism signals to your body that a foreign organism is present and that it must be removed.
There are two main types of effector T cells: cytotoxic and helper T cells.
Cytotoxic T cells kill your own cells if they are infected for example with SARS-CoV-2.
Helper T cells produce chemical substances, that activate, attract, and regulate other immune cells, including B cells.
The adaptive immune system remembers earlier infections
The adaptive immune system is termed so because it adapts by remembering earlier infections that you have had. This feature is possible due to memory T and B cells.
The great advantages of your memory cells are that they are long-lived, easy to activate, and recognise the same antigen as your effector T and B cells.
If the same microorganism happens to infect you again, your memory cells will quickly get activated.
Following reactivation, your memory cells initiate an immune response, which is more efficient than first time you encountered the microorganism. Your immune system has adapted, and you will most likely not fall ill before your immune cells have eradicated the infection. This concept is called immunity.
When microorganisms mutate, they can escape your immunity
The ability to develop immunity via memory cells is the reason why vaccines work. (Read more under Facts: How vaccines work). This however begs the question, why do we need new vaccines such as the flu vaccine every year?
This is because influenza mutates. When the virus mutates, its antigens change, and your pre-existing memory cells will no longer be able to recognise it.
Different microorganisms mutate with varying degree. This explains why you may lose immunity against some infections, whereas immunity against other infections lasts your entire life.
The influenza is a fast mutating microorganism. In comparison, SARS-CoV-2 only mutates at half the pace of influenza.
This suggests that immunity against COVID-19 will last for a while. However, scientists are still trying to determine how long you might be immune.
How to expand our knowledge about the immune system and COVID-19
Even though we already know a lot about the immune system, many questions remain unsolved.
You may have read elsewhere, that some patients lack good antibodies against SARS-CoV-2 even though they have had COVID-19, and that scientists are in doubt whether these patients are immune to SARS-CoV-2.
Fortunately, new research shows that some patients with few antibodies instead have many memory T cells against SARS-CoV-2.
Some studies even suggest that some people have memory T cells able to recognise SARS-CoV-2 without ever having COVID-19.
Scientists believe that the SARS-CoV-2-specific memory T cells have arisen, because these people have had a normal cold caused by a virus related to SARS-CoV-2.
Since the two viruses resemble each other, it is possible that some memory T cells can recognise both viruses. Whether these memory T cells result in immunity to COVID-19, is still unknown, but it is being investigated.
A pandemic like COVID-19 emphasises why we continuously need research in the field of immunology (studies of the immune system).
The better we understand how the immune system works, the better we can design innovative therapies that can prevent and treat both infections like COVID-19, but also autoimmune diseases (diseases where your immune system mistakenly attacks your own body) and cancer.
Read the Danish version at Videnskab.dk's Forskerzonen.
References:
Julie Hagedorn Thomsen's profile (LinkedIn)
Kristoffer Haurum Johansen's profile (ResearchGate)
Klaus Okkenhaug's research group, University of Cambridge
Carsten Geisler's research group, University of Copenhagen
Pamela L. Schwartzberg's research group, National Institutes of Health









