This article was produced and financed by The Research Council of Norway

Few regular users of strong painkillers
Few Norwegians take opioids such as Paralgin forte and morphine regularly. Those who do, however, use these strong painkillers over extended periods.
Denne artikkelen er over ti år gammel og kan inneholde utdatert informasjon.
Each year roughly 10 per cent of the Norwegian population are given a prescription for opioids. Until recently, the number of these who can be considered regular users of such medications was unknown.
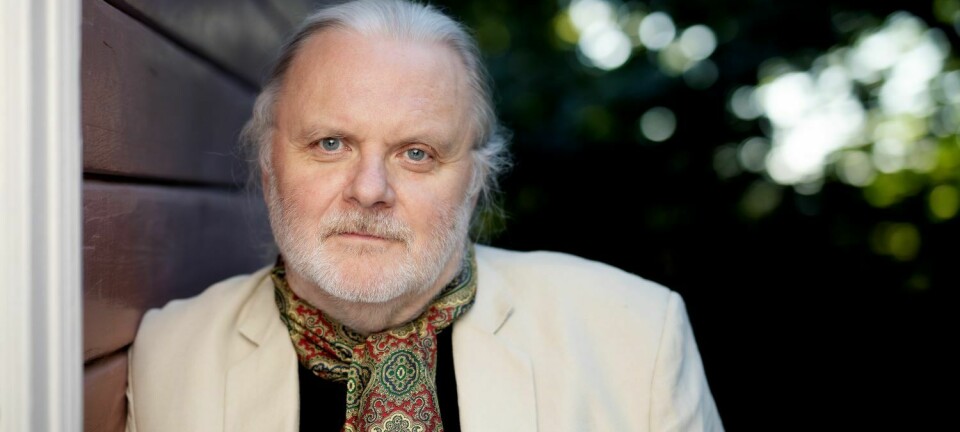
“We now know we are talking about approximately one per cent of the overall Norwegian population, which is not a particularly worrisome figure,” believes Kristian Svendsen, a doctoral research fellow at the Norwegian University of Science and Technology (NTNU) in Trondheim.
“I think many physicians, pharmacists and others have overestimated the proportion of regular users.”
Opioids alleviate pain and suppress coughing. Codeine, an ingredient of Paralgin Forte and Pinex Forte, is by far the most used opioid in Norway. Morphine, tramadol and oxycodone are also commonly used opioids. The trouble with opioids is that they can lead to strong side effects and dependency.
Physicians more cautious than thought

Petter Borchgrevink of St. Olavs Hospital’s National Competence Centre for Complex Symptom Disorders is heading the project studying Norwegians’ use of opioids. The project receives funding under the Research Council of Norway’s Programme on Alcohol and Drug Research.
“In the USA, painkiller abuse is considered the second-most pervasive substance abuse problem, after cannabis. This is one of the reasons that many people are worried about widespread dependency on Paralgin forte and opioids in Norway,” explains Dr Borchgrevink.
In his doctoral research, Kristian Svendsen developed advanced methods for measuring the use of opioids in different population groups. Now he has found that Norwegian physicians are more conservative about prescribing these drugs than was previously thought.
Only 0.16% use opioids round the clock
Svendsen studied figures from the Norwegian Prescription Database for the period 2004-2008. In this record of all prescriptions dispensed to private individuals in Norway, each prescription is matched to its patient, making it possible to see how many prescriptions an individual has had filled.
The majority of the roughly 500 000 Norwegians per year who took opioids received only one prescription. Many received two to three, after a broken bone or an operation, for example. Over 100 000 persons had more than three prescriptions filled, but only a small proportion of these could be categorised as year-round users of opioids.
“Applying strict definitions,” continues Svendsen, “we found that at the end of 2007 just 0.16 per cent of the Norwegian population were using opioids round the clock, while one per cent were using opioids at least half the days in a one-year period.”
Many with chronic pain
Svendsen’s research indicates that patients who regularly use opioids tend to use them over an extended period of time; three years after the study began, seven of 10 users were still receiving treatment with opioids.
On average, regular opioid users take them for 14 years. Svendsen cautions against automatically defining this use as problematic dependency, however.
“These patients may be dependent on their medication, but there is nothing necessarily wrong with that. We know that roughly three out of 10 Norwegians report suffering from chronic pain. Some of these are dealing with intense pain – which may help to explain the long-term use of painkillers.”
Morphine may be preferable
All regular users of such drugs need to be followed up closely. Physicians must be aware of the risks of side effects and dependency, and continually assess whether patients are receiving the best treatment.
“Paralgin Forte and Pinex Forte are not an optimal treatment,” asserts Svendsen. “First, they are short-acting, so that patients must often take new tablets. Second, not everyone receives the full effect of this treatment.”
One in 10 patients, in fact, cannot convert the active ingredient codeine to morphine. The resulting medicinal effect is roughly the equivalent of taking paracetamol (acetaminophen), but with the added drawback of side effects.
“Physicians have an ingrained scepticism about switching to medications stronger than Paralgin Forte or Pinex Forte. But for some patients,” says Svendsen, “particularly those with intense chronic pain, it would be better to prescribe stronger, longer-acting medications such as morphine.”
Translated by: Darren McKellep/Carol B. Eckmann