This article was produced and financed by The Research Council of Norway
Towards personalised cancer treatment
An extensive research project will examine the errors occurring in the genes of several thousand Norwegian patients. The objective is to develop treatment that is better adapted to the individual patient.
Denne artikkelen er over ti år gammel og kan inneholde utdatert informasjon.
Even though all cancers are caused by gene aberrations (mutations) in the DNA of normal cells, each tumour is unique.
Each type of cancer comprises a number of subgroups characterised by different mutations. Since mutation processes are random the mutations that take place in each patient, and even in different cells in the tumour, will differ.
When it comes to treatment, however, most patients are given largely the same regimens. This may be highly effective for some patients while the benefit to others is slight. And some may be so unfortunate as to experience nothing but the side effects.
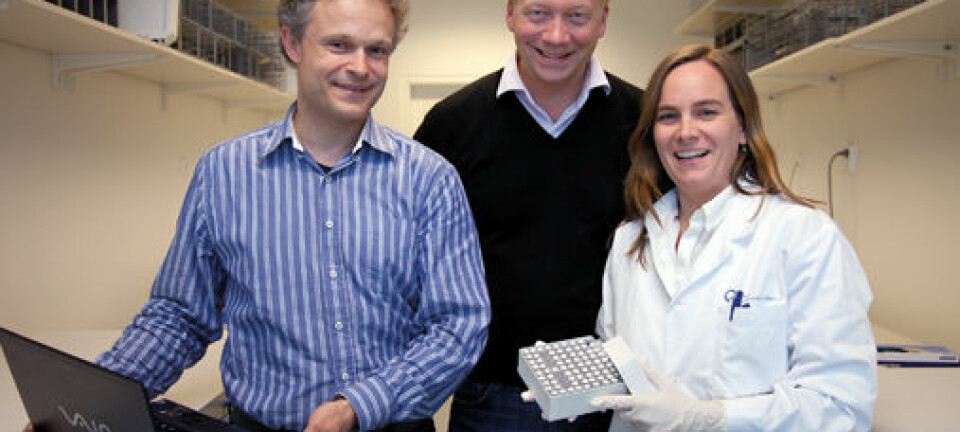
“One fundamental problem is that the various patient groups have not been categorised adequately. The causes of cancer are far more complicated and complex than we knew,” says Ola Myklebost, senior researcher at Oslo University Hospital and professor in the Department of Biosciences at the University of Oslo.
Sequencing every single gene
Myklebost is heading a comprehensive project co-funded under two of the Research Council of Norway’s programmes: the Programme for Publicly-initiated Clinical Cancer Studies (KREFT) and the Research Programme on Biotechnology for Innovation (BIOTEK2021).
Using “next generation” gene sequencing, the researchers are first going to examine mutations in all genes in patients suffering from eight different types of cancer: melanoma, breast cancer, colorectal cancer, lymphoma, prostate cancer, sarcoma, leukaemia and myeloma. More studies will be added as the project progresses.
“We want to find out which mutations are distinct in various cancer types and what effect these mutations have. This is an essential starting point for developing and employing personalised treatment far more widely than is the case today,” Myklebost says.
Teaming up with Myklebost on the project are researchers and physicians from throughout all the regions of Norway. Initially, the researchers were to sequence 1000 genes from the blood and tumours of each patient. The plans have since been expanded and the researchers are going to look at all of the roughly 22 000 genes.
New sequencing machines that are capable of analysing all genes at once at ever increasing speeds are being developed non-stop, and they are becoming less and less expensive to operate.
"In our work we will be using a machine that is ten times faster than the last one we had. The degree of sequencing we are now planning would simply not be possible with the machine we purchased just three years ago,” Myklebost explains.
Laying the foundations for personalised treatment

Numerous studies in recent years have shown that it is wrong to consider one type of cancer as a single, more or less homogeneous illness. For example, Norwegian cancer researcher Anne-Lise Børresen-Dale and her partners at the Oslo University Hospital have shown that at least ten different kinds of breast cancer exist. It is clear that treatment needs to be adapted to the specific type of cancer as well as to the individual patient.
Myklebost points to lung cancer as a cancer where personalised treatment is being applied.
“Lung cancer researchers are now examining specific mutations in the cancer cell genes that provide a foundation for targeted therapy. A certain mutation found in approximately four per cent of the tumours is responsive to a medicine developed to block this particular pathway. Patients with this type of tumour react well to treatment,” the professor explains.
“Unfortunately, there are so many different mutations in the tumour cells that clones arise that do not respond to the medication. These clones eventually gain the upper hand and the effect of the medication diminishes over time,” he adds.
In some cases second line treatment is available, in others a new mutation profile may reveal more options.
Genetic aberrations across cancer types provide clues
Up to now, the common procedure has been to select medicines and treatment based on the organ affected by cancer. It turns out, however, that many of the same gene aberrations appear across different types of cancer.
This is a very positive finding, Myklebost believes, for instance with regard to rare forms of cancer where the development of disease-specific treatments is not very profitable for the pharmaceutical industry.
“By finding common features between these rare types of cancer and cancers for which medications exist, we may be able to develop new treatment options. One advantage to applying medications already in use for one type of cancer in a new area is that the side-effects are already well known,” Myklebost asserts.
Tailoring treatment for each individual patient
The researchers still do not know any single mechanism that is fundamentally responsible for the growth of cancer tumours.
As they discover the mechanisms, medications adapted to those specific gene mutations will have to be developed. For the time being, targeted treatments are only available for a handful of patients and at high cost.
There are also many technical, ethical and legal challenges that have to be overcome before personalised treatment becomes a standard part of health services.
“One of the major challenges is documenting the effect of a treatment that is only suitable for a few patients. Classic trials on a large number of randomised patients will of course be impossible,” Myklebost points out.
Still, he remains optimistic.
“In coming years diagnostics will steadily improve and become more precise. Gene-sequencing of cancer tumours on a moderate scale may be cost-effective already or will be so in the near future,” he concludes.
Translated by: Glenn Wells/Carol B. Eckman