New imaging technique predicts efficiency of cancer treatment
Scientists have found a new method for assessing whether aggressive brain cancer can be treated with drugs. With the new technique, pictures of the chaotic network of blood vessels in tumours can reveal whether the patient will live longer with treatment.
We are now one step closer to understanding the most aggressive form of brain cancer, glioblastomas.
Without treatment, many patients only survive a few months, while those in treatment can live for about 18 months.
For some patients, however, treatment does not have much of an effect, but physicians have so far found it difficult to identify these patients.
Researchers from the US and Denmark have now developed a new imaging technique that gives a more accurate picture of how the architecture of blood vessels in brain tumours is affected by medication. This makes it easier for physicians to assess whether the treatment will work or whether another form of treatment should be used.
With the new imaging technique we can calculate what blood vessels in the tumour look like, and this assessment allows us to assess fairly accurately whether treatment will increase the patient’s survival time.
“With the new imaging technique we can calculate what blood vessels in the tumour look like, and this assessment allows us to assess fairly accurately whether treatment will increase the patient’s survival time,” says Associate Professor Kim Mouridsen of the Institute of Clinical Medicine at Aarhus University, Denmark.
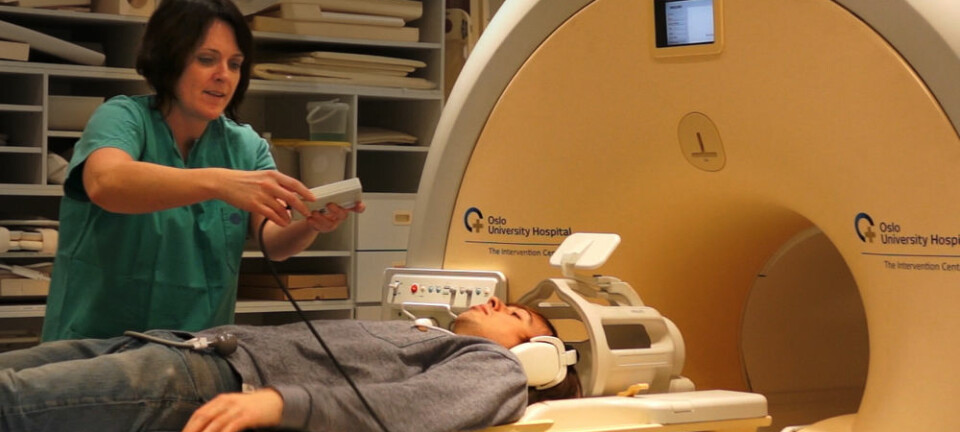
New way of using MRI scanners
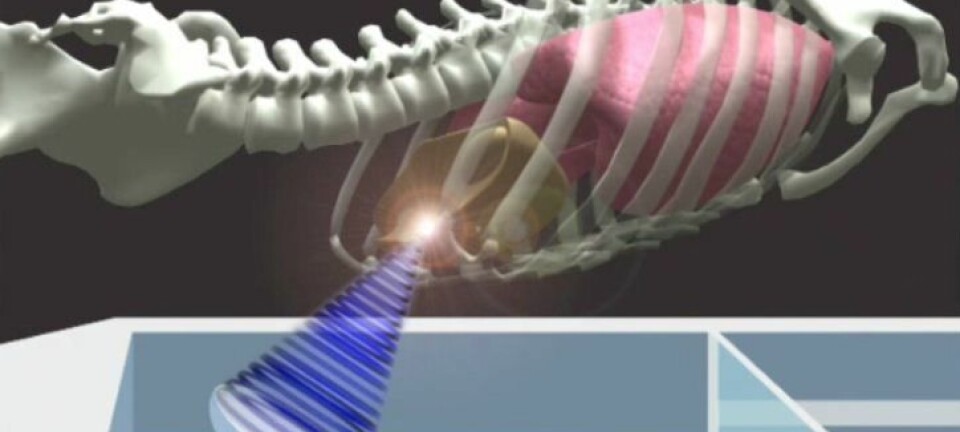
Mouridsen, who heads the Neuroimaging Methods research group, has helped develop a mathematical structure that can be integrated into a regular MRI scanner.
In simple terms, the researchers use mathematics to convert the signals coming out of an MRI scan into curves that rotate either clockwise or counter-clockwise in a system of co-ordinates.
When the curve rotates clockwise, it means that the tumour has many strange, ineffective blood vessels.
These odd-looking blood vessels are an indication that the tumour lacks oxygen, and oxygen-deficient tumours are dangerous because they are harder to treat.
An oxygenated tumour is easier to treat
Treatment usually consists of medication that inhibits the growth of new blood vessels.
This shrinks the tumour and makes it less oxygen deficient because the blood vessels become more effective. When the tumour receives oxygen, the efficiency of chemotherapy and radiation therapy increases.
This enables doctors to not only shrink the tumour, but also to increase the chances of keeping the disease at bay with conventional cancer treatments.
Method can predict who will live longer
Not all patients, however, respond to the blood-vessel growth inhibitor.
With the new imaging technique, the researchers could, after only a few weeks, predict whether or not the medicine would prolong the patient’s life.
Patients whose tumour blood vessels started to normalise within a month survived an average of 341 days, while those whose tumour blood vessels did not normalise lived an average of 146 days.
”We have now come one step closer to understanding why the drug does not work on all patients,” says Mouridsen. “We have also found a way of predicting whether the treatment will work. Then we can start up another form of treatment for those patients who do not respond immediately.”
------------------------
Read the Danish version of this article at videnskab.dk
Translated by: Dann Vinther