Researchers' Zone:

Cancer-seeking 'missiles' may be the future weapon against breast cancer
The pH around a tumor is often different from the rest of the body. We can use this to develop antibodies that work like cancer-seeking missiles.
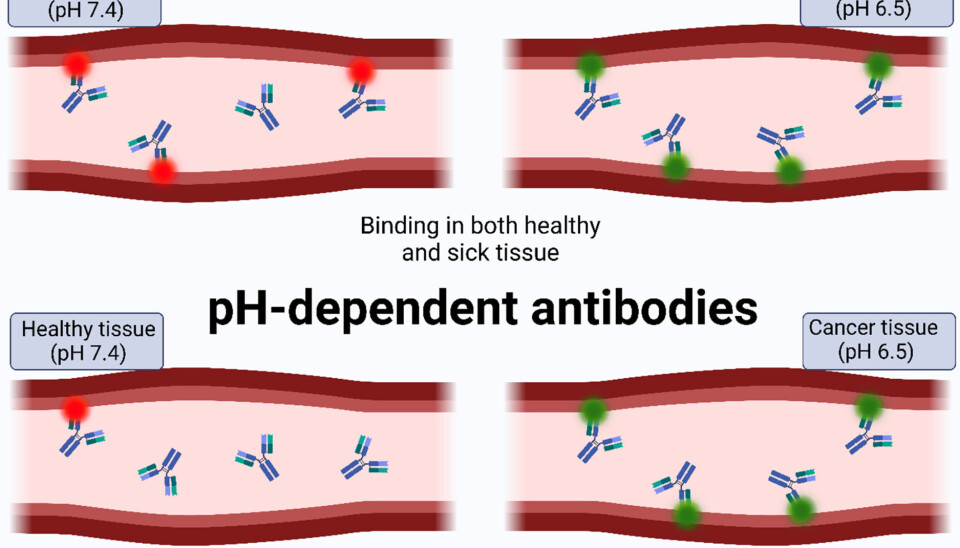
A new strategy to optimize medicinal antibodies may be underway, namely the use of engineering to transform conventional antibodies into pH-dependent antibodies.
These antibodies bind depending on the pH-value of the cells they are designed to target. For example, they could act as cancer-seeking missiles inside our body, distinguishing between tumor sites and healthy tissue that have different pH values.
But what makes these antibodies so effective, and what role could they play in the battle against diseases like breast cancer in the future?
From body to laboratory
Antibodies can be produced not only in our bodies during immune responses, but also in laboratories for medical use when we get sick, and our bodies cannot cope on their own.
These lab-made antibodies, known as monoclonal antibodies, work just like the antibodies found in our bodies and have been used as therapeutics since 1986.
Monoclonal antibodies are used to treat a range of complex diseases, including autoimmune diseases, sclerosis, cystic fibrosis, infectious diseases like covid-19, and not least a range of cancers.
An example is Herceptin, an antibody used to treat breast cancer.
With breast cancer alone being responsible for hundreds of thousands of deaths annually (see here and here), it is important that we have the best treatments available for this devastating disease.
Room for improvement
While a monoclonal antibody like Herceptin is already able to treat breast cancer, there is still room for improvement.
Treatment with Herceptin can have unwanted side effects like targeting healthy heart muscle cells, which can lead to heart damage (see here and here).
If it were possible to make Herceptin work mainly in breast cancer tumors, the treatment would not only be more effective, but the risk of side effects would also be reduced.
But how could this be done? To answer this question, we first need to understand how the immune system responds to cancer cells and how they can be identified.
Identifying a cancer tumor
Your body regularly fights potentially cancerous cells before they reproduce without you even noticing.
However, the immune system is not always able to distinguish cancer cells from healthy cells, which is one of the reasons why a disease like breast cancer is so difficult to treat.
The environment around a tumor tends to be more acidic, which can expose cells as possible cancer cells.
While healthy tissues have a pH value around the so-called physiological pH level of 7.4, many tumor sites have a pH value of 6.5 or lower (see here and here).
Transforming antibodies into cancer-seeking missiles
By engineering antibodies to be able to detect this difference in pH, they will only bind to their antigens when they are displayed on tumors.
This would potentially increase the ability of the antibodies to specifically target tumor cells while not attacking any healthy cells.
Such antibodies would work like cancer-seeking missiles within our body, defending the body by only attacking tissues when they detect a low pH-value and thus the presence of cancers.
Tumors take control of our body’s internal machinery
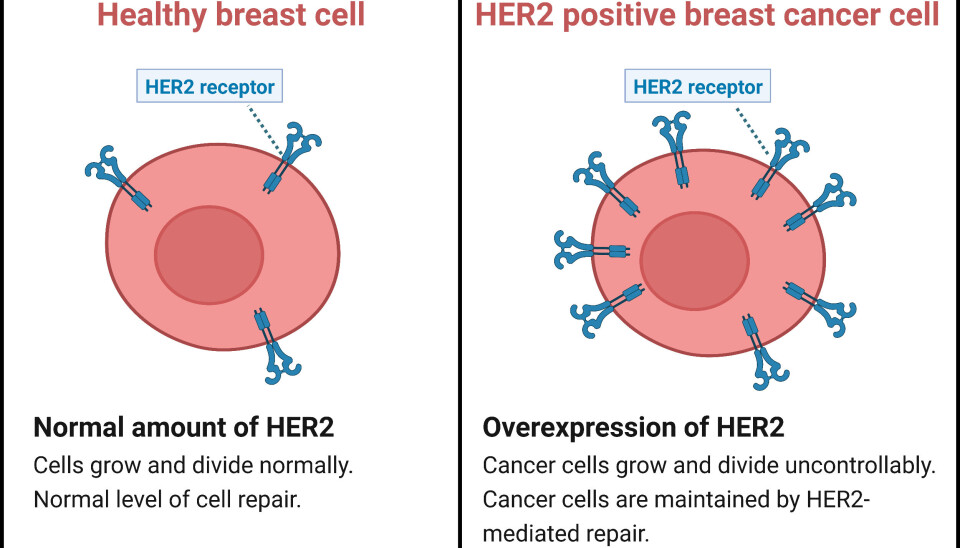
In treatment of breast cancer, Herceptin works by targeting HER2, a protein associated with breast cancer that helps the disease develop.
This makes HER2 a well-suited target for current and future therapy even though HER2 is also present in healthy tissues in our bodies.
There, HER2 has various important functions such as promoting cell growth and repair, like a gardener tending to a broad range of beautiful plants.
However, in some cases HER2 is not a very smart gardener and is not always able to distinguish between weeds and the beautiful plants in the garden.
This illustrates how a natural protein like HER2 is associated with breast cancer: tumors are able to take advantage of the good intentions of the gardener HER2, helping the cancer to develop and spread throughout the body, like weeds in a garden.
In this way, tumors are able to take control of the internal machinery of our bodies, underlining the importance of developing and engineering the right weapons like antibodies to effectively fight cancers.
Developing pH-dependent antibodies
Antibodies are developed and engineered through antibody discovery.
Of the many antibody discovery methods available today, a popular example is the 2018 Nobel Prize-winning technology called phage display, which allows millions of antibodies to be tested simultaneously.
Furthermore, phage display makes it possible to assess whether antibodies can bind to a specific target under different conditions, such as different pH values.
This unlocks the potential to develop antibodies that act like cancer-seeking missiles:
They attack cancer-related proteins at tumor pH (6.5), while leaving the same proteins in healthy tissues alone, thus obtaining a more specific cancer treatment than current approaches.
Challenges in targeting tumors
Sounds easy, right? Unfortunately, the reality of developing new treatments is not always as simple as the theory.
Countless factors need to be considered before delivering treatments into the body, and antibodies with pH-dependent antigen binding are no different.
The risk of targeting healthy tissues in the body remains a challenge as there are a variety of different pH-levels in the body.
For example, our digestive system have pH values of 6.5 and lower, underlining the risks of side effects.
Furthermore, tumor sites are complex and do not always have the same pH-values, meaning that more experiments simulating the human body are needed before the technology can be used in therapy.
A treatment strategy of the future
However, the technology is being tested rapidly, and therapeutic antibodies with pH-dependent antigen binding already exist, such as so-called sweeping antibodies.
These antibodies have the opposite pH-binding effect, where they bind well at physiological pH, while binding poorly at lower pH.
It therefore seems realistic to obtain pH-dependent antibodies with tumor pH targeting properties as well.
The technology of selectively targeting breast cancer and cancer in general, could be a great improvement to current cancer therapies, reducing the side effects of cancer treatments, and potentially allowing dose-increases for more effective treatment.
This makes the future for new generations of cancer treatments looks brighter than ever.
Sources
- Jakob Weimann's profile (LinkedIn)
- Nick J. Burlet's profile (DTU)
- Christoffer V. Sørensen's profile (DTU)




