A study on Irritable bowel syndrome resulted in improvement for 90 percent of patients, then their funding ran out
The Norwegian Patient Association started a fundraising campaign for a Norwegian research project on faecal transplants to treat Irritable bowel syndrome (IBS).
In a November 2019 article, Marte Rykkje Halstensen shared how her life changed radically after participating in a study at Stord Hospital in Vestland county.
Halstensen received a dose of transplanted faeces from a healthy donor into her intestine –called a faecal transplant. Within a few weeks, she went from struggling with constant abdominal pain, constipation and a bleeding bowel to being healthy.
Halstensen was just one participant in a study in which almost 90 percent of the participants experienced improvement and almost 50 percent fully recovered. The results of the study were published in the scientific journal Gut in 2020.
The study results did not go unnoticed.
Two researchers in Nature Reviews: Gastroenterology & Hepatology commented that the results from a new study suggest that faecal transplantation can be an effective treatment for irritable bowel syndrome (IBS).
In The Lancet: Gastroenterology & Hepatology, Stord's results were described as impressive.
But the commentators note an important point.
“We don’t know why the transplantation worked so well in the study at Stord. This will be important to find out.”
Very divergent results
A handful of studies on faecal transplant for IBS have been carried out previously. The results are divergent, to say the least.
In one case, the placebo group actually had better results than patients who received the real treatment. Other studies have shown modest improvements.
Part of the explanation for these large differences may be that researchers do not currently have a standardized method for administering the transplants. The research field is in its infancy, and researchers have to experiment their way forward.
Some researchers use one faecal donor. Others mix faeces from several donors. Some administer one dose, while others give more. In some experiments, the new intestinal flora are inserted into the colon. Other participants swallow capsules that dissolve in the intestinal system.
All of these choices can affect the results and could thus be part of the secret behind possible success.
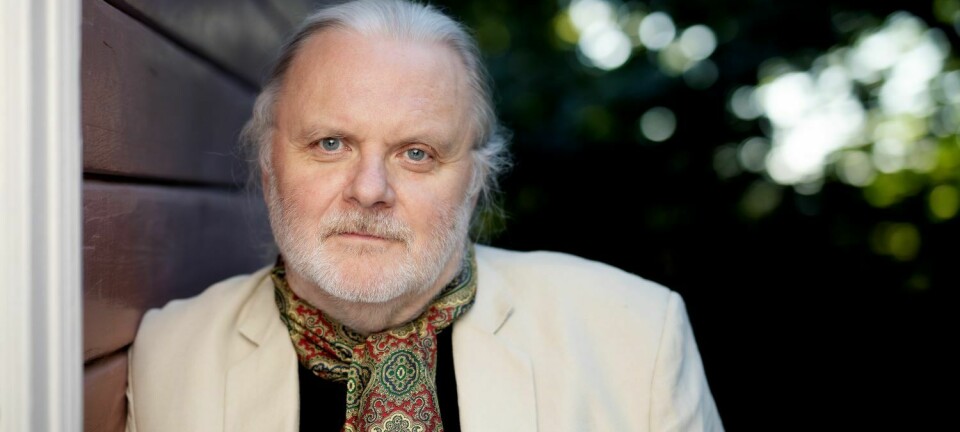
Therefore, says Magdy El-Salhy, “it’s extremely important to do further research on this potential treatment.” He is a professor at the University of Bergen, the chief physician at Stord Hospital and heads the study on faecal transplantation.
Golden opportunity
“We’ve been given a golden opportunity here,” says El-Sahy.
“We were lucky and got good results, and now we have to find out which factor was responsible.”
He believes that the donor could play an important role. In the experiment at Stord, they used a very carefully selected super donor, with excellent health and intestinal flora. But other factors might also come into play.
“For example, our donor freezes the stool and delivers it frozen,” El-Salhy says.
This could be important, because many of the bacteria in the gut cannot tolerate being in the air for very long. Maybe more bacteria would survive if they were frozen immediately.
El-Salhy inserts the intestinal flora into the upper part of the intestine, via a gastroscope that is passed through the stomach and down to the beginning of the small intestine. The transplant location might also be a factor.
Does the small intestine play a role?
IBS is usually mostly associated with the colon. A few decades ago, it seemed perfectly clear that the colon was where the bacteria were located. The small intestine and stomach were considered practically sterile.
However, the lack of bacteria in the small intestine may have other causes, El-Sahly says.
“A lot of bacteria in the small intestine are anaerobic. They die in the air and we can’t cultivate them.”
But new techniques for DNA sequencing have shown that the small intestine is not free of microbes at all.
"It could be that bacteria in the small intestine are more important than we think," says El-Salhy.
Now he worries that they’ll never find out what was responsible for the results of the study at Stord Hospital.
The project is not receiving funding to continue the research.

Worth supporting, but not prioritized
El-Salhy has applied for research funding from both Helse Vest and the Research Council of Norway. Both applications were rejected.
The project is considered worth supporting, but an overall assessment concluded that the research project did not achieve sufficient priority to qualify for support, Helse Vest wrote in its justification.
Research director Renate Grüner from Helse Vest states that the decision is not about downgrading IBS.
“No areas are considered more or less important than others. But there’s a lot of competition for the available funds,” Grüner says.
Project applications are assessed according to scientific quality and clinical benefit. Of the 276 projects that applied for support, only 54 were awarded funding.
“As in previous years, this time the applications were again of very high quality. This doesn’t mean that rejected projects are not eligible for support,” Grüner says.
“The project in question previously received support from Helse Vest – from 2018 to 2020 it received a total of NOK 3.6 million. Not reaching the final round this time is simply due to the fierce competition for a limited pot of research funding,” Grüner writes.
Patients have started a fundraising campaign
However, the funding rejection has provoked strong reactions, both among patients who received help through the project and the National Association for Digestive Diseases (LMF).
“Today's treatment options are a big vacuum that needs to be filled. It’s unfortunate that a promising research project has to end when it shows positive results for 90 percent of patients, and where one in five Norwegians falls into the target group,” says Mads Johansson, general secretary of LMF according to the association's website.
The association has started a fundraising campaign to raise money for the project. They have now collected approximately NOK 130 000 (~EUR 13 000).
Politicians have also taken action.
Helge André Njåstad from Norway’s Progress Party (FrP) told LMF that several voters in his district alerted him to the situation. On 19 April, Njåstad submitted a written question to the Minister of Health and Care Services, Bent Høie, asking whether the Minister would take the initiative for the project to continue.
“My answer to that is that I neither initiate nor directly fund research projects. Funding decisions are the responsibility of the regional health authorities,” Høie replied.

Rejections not uncommon
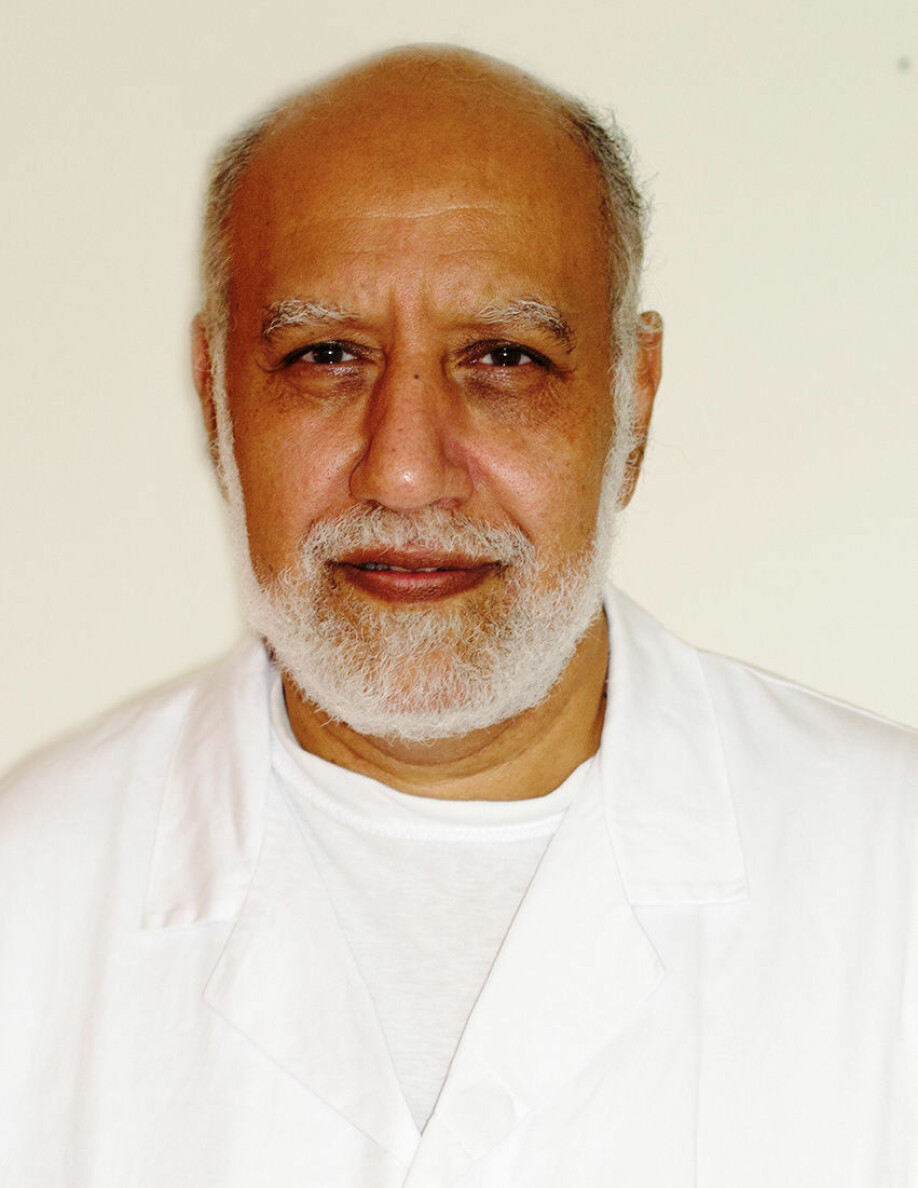
Rasmus Goll at UiT Norway’s Arctic University is also researching faecal transplantation for IBS at the hospital in Harstad municipality. He was recently awarded funding for a large project that will recruit patients from several places in the country.
But Goll says that application rejections for research funding are commonplace for researchers.
“That’s how research funding works – you get ten rejections for every time you receive funding,” he says.
“I can understand that they’re disappointed about not getting money, but they just have to apply again next year.”
Goll thinks it might have been particularly difficult to get funding this year. So much research has focused on COVID-19, and this might have shrunk the funding pot for other projects.
However, Goll agrees with El-Salhy that investigating which factors contributed to the results at Stord is an important next step.
Goll is curious about the potential significance of having some of El-Salhy's patients repeat the treatment. In his own study, Goll observed that both patients who got better from the faecal transplant and those who did not experienced changes in their intestinal flora.
Was the change perhaps just too small in the patients who did not improve?
Goll wonders if the success rate would improve if patients were given more than one treatment.
Need several million
El-Salhy is moved by the fundraising campaign under the auspices of LMF.
“We’re grateful for everything that is raised and will do what we can with the funds we have. The fundraising is symbolic and reminds us that patients have a say.
But a lot of money is needed to keep such a project going. El-Salhy estimates the research team will need NOK 1.5 million a year over the next five years. He will soon be retiring but is very keen to further support younger researchers.
“I have colleagues here at Stord who would like to continue the project,” he says.
“We’ve spent 15 years building up the research environment here. We now have experience, facilities, systems and lists of 1 500 patients who could participate in the studies. It would be pointless to throw it all away.”
“My goal is for the project to continue until we have more background and until we have a documented treatment,” he says.
Translated by Ingrid Nuse
Read the Norwegian version of this article on forskning.no.