Resistant bacteria can be tamed again
Pioneering research has found the key to making resistant bacteria sensitive to antibiotics. New medicine could be on the market within two years.
Researchers have developed a new drug that can cure tens of thousands of patients around the world who have been infected by otherwise untreatable bacterial infections such as staphylococci, tuberculosis or salmonella.
The drug could well be a revolution in the fight against multi-resistant bacteria – a fight that mankind appeared to be losing.
A Danish research group has just been granted a patent for the medicine, which makes resistant bacteria susceptible to antibiotics again. This means that patients can be cured using ordinary antibiotics that the bacteria have become immune towards.
The drug has already been shown to be effective against resistant tuberculosis, multi-resistant staphylococci (MRSA) and resistant salmonella-typhoid bacteria.
Schizophrenia drug paved the way
The key to the breakthrough was found in a drug traditionally used to treat schizophrenia.
“We’ve known for a long time that psychoactive (psychopharmacological) drugs have an antibiotic effect,” says one of the researchers behind the new discovery, Oliver Hendricks, a postdoc at the University of Southern Denmark (SDU). “We have now separated the mechanism of that effect from the rest of the drug, and the result is a product that can make resistant bacteria sensitive to antibiotics again.”
Drug smashes bacterial pump
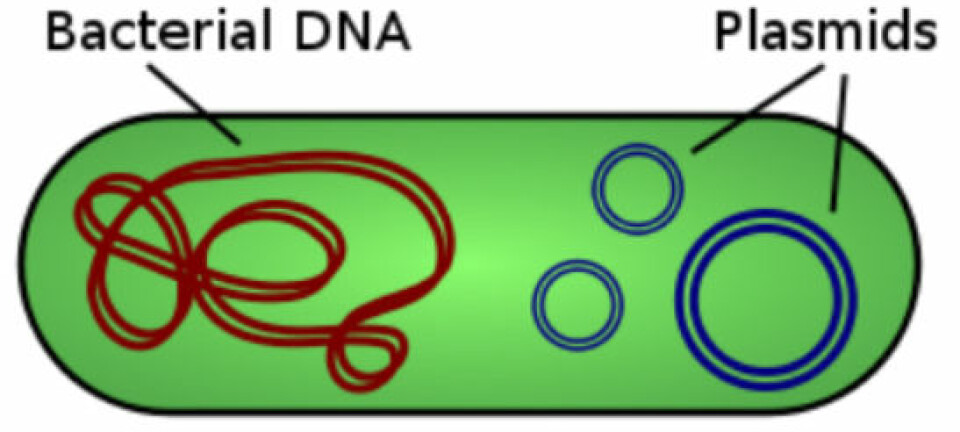
Bacteria’s resistance arises from several causes. One of the common forms of resistance is a so-called efflux pump. This pump, found in the outer cell membranes of bacteria, is designed to pump antibiotics out of the bacteria cell so the antibiotic never acts on the bacteria.
The drug, JEK47, affects the outer cell membranes of the resistant bacteria, preventing the efflux pumps from working correctly. The bacteria can no longer pump antiobiotics in the cell out again. JEK47 must be followed by treatment with ordinary antibiotics that, with the help of the new drug, can kill bacteria that prior to the treatment were resistant to antibiotics.
“We’ve also discovered that JEK47 works against other forms of resistance that do not involve efflux pumps,” says the researcher. “However, we have yet to investigate the mechanism behind that effect completely, but we are convinced that there is also a change in the bacterial membrane structure in these cases.”
Already tested on bacteria, animals and humans
Researchers started studying non-antibiotics – ways of making resistant bacteria sensitive to antibiotics again – in 1976.
So far, the effects of JEK47 have been documented against staphylococci and salmonella in mice, while Argentinean researchers have shown that the drug thioridazine – the origin of JEK47 – works on patients with multi-resistant tuberculosis.
“We are very pleased that our international partners have confirmed the effect of our drug,” adds Hendricks. “Because of the great weight of the test results, we are certain that our medicine works.”
Greatly reduced side-effects of psychoactive drugs
Psychoactive drugs are known for their serious side-effects, but the extraction of JEK47 from the original drug, thioridazine, has greatly reduced the side-effects.
“We removed the part of the drug that affected the brain, thereby removing 80-85 percent of the side effects,” adds Hendricks.
JEK47 has been thoroughly tested and is now approved as medication for combination treatment against resistant bacteria in Europe.
Hendricks hopes JEK47 can be on the market in one to two years.
Criticism
The new medicine has come under fire, partly because Thioridazine – the origin of JEK47 – has been documented to have serious side effects such as heart complications and in rare cases even death.
Hendricks understands these worries, but he feels there is still a need for the new drug:
“We’re perfectly aware that JEK47 can be toxic, but studies have shown that it only causes death in 5-8 patients out of 10,000 treatments – and this is almost exclusively restricted to people aged 50 or over,” he says.
Hendricks and his colleagues are backed up by Luca Guardabassi, an associate professor at the Department of Veterinary Disease Biology at the University of Copenhagen:
“The European Center for Disease Prevention and Control (ECDC) estimates that approximately 25,000 people die every year because of resistant bacteria,” says Guardabassi. “Many of these people could benefit from a drug against the resistance of antibiotics even despite the possible side effects.”
Translated by: Michael de Laine
Scientific links
- Reversal of resistance in microorganisms by help of non-antibiotics
- Potential role of non-antibiotics (helper compounds) in the treatment of multidrug-resistant Gram-negative infections: mechanisms for their direct and indirect activities