Sleeping pills can double risk of traffic accidents
The risk of getting involved in a traffic accident is twice as high within a week after filling out a prescription for some of the most popular sleeping pills.
Denne artikkelen er over ti år gammel og kan inneholde utdatert informasjon.
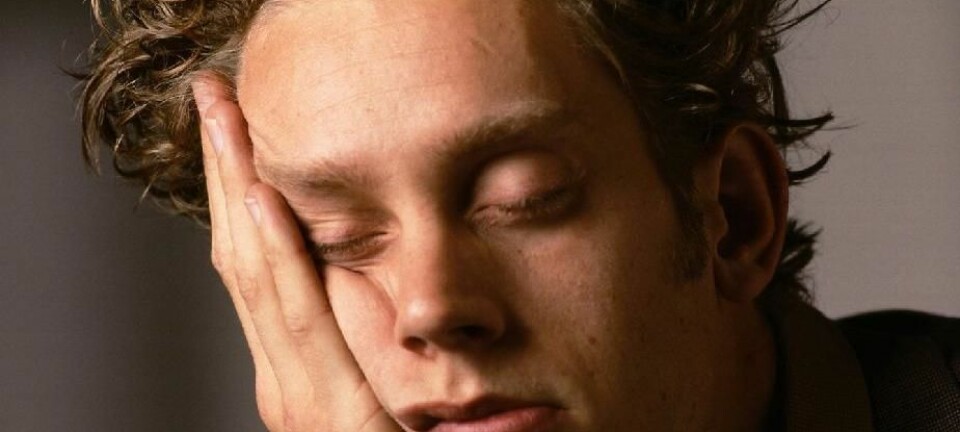
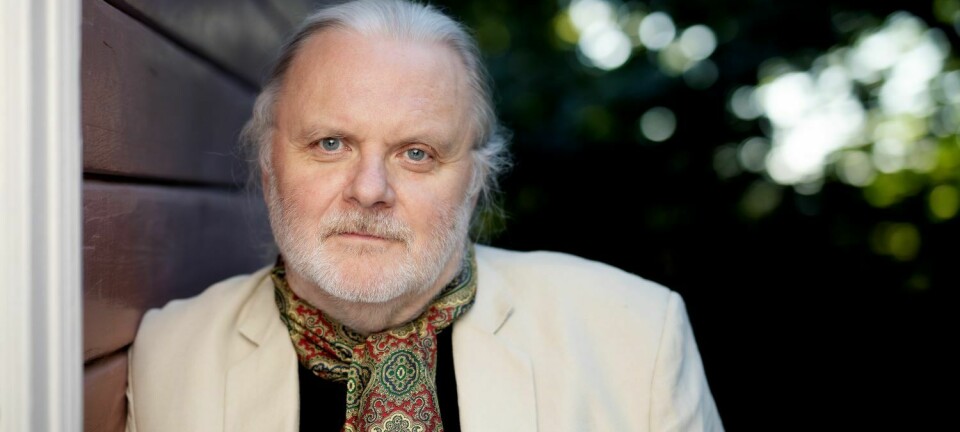
“The first days after people buy prescribed sleeping pills at a chemist’s they run a bigger risk of getting into a traffic accident,” says Ingebjørg Gustavsen.
Gustavsen is a physician who has worked for years studying drugs and intoxicants at the Norwegian Institute of Public Health (FHI). Now she works with clinical pharmacology at Ullevål University Hospital in Oslo.
She has no definite proof but her research indicates the rise in risk is linked to increased usage of the pills right after a prescription for them has been filled.
In work on a recent doctoral dissertation she analysed sales of prescription sleeping pills at pharmacies and the frequency of traffic accident involvement among persons who had bought the pills.

She looked at issue of the following medicines for insomnia – often referred to as the Z-drugs:
- Imovane (zopiclone)
- Stilnoct (zolpidem)
- Alopam (nitrazepam)
- Rohypnol (flunitrazepam)
The risk of traffic accidents rose with all these Z-drugs, but the link was strongest with zopiclone, which in Norway is sold under the brand name Imovane.
“We found a double risk of involvement in a traffic accident the first week after a person purchased zopiclone at the drug store,” says Gustavsen.
This was in comparison with any person who did not get the prescription filled in the same period.
The researcher says this is a commonly used drug.
Annually used by 300,000
“In Norway there are over 300,000 who used it at least once every year. This is actually in fifth place among the most sold prescription drugs in Norway,” says Gustavsen.
Zopiclone is a sleeping pill recommended to persons with short-term insomnia problems.
“But research reveals that lot of people use it long-term, often for years,” says the researcher.
The older the patients, the more prevalent was their use.
“Women use it more than men and it is prescribed to a third of all women aged 80 in Norway,” she says.
Maximum blood levels
If you drink alcohol and get behind the wheel in Norway you are in trouble if you get caught with a blood level of 0.02 percent.
Last year the road laws incorporated comparable limits with regard to various prescription drugs.
However, these limits do not apply when the driver has a prescription for the drug.
New law does not apply to legal use
The results of Gustavsen’s doctoral thesis work have already led to changes in Norway’s traffic laws.
In addition to the limits on alcohol levels in the blood, maximum levels have been stipulated for 20 other substances, including zopiclone.
“But the limits are only for abuse of the drugs. If you have a prescription and can prove it, these limits don’t apply,” says Gustavsen.
That does not mean people can drive all they want after downing prescribed medicines, but the limits are not as explicit when drivers have used drugs prescribed to them by doctors.
If you have such medicines in your bloodstream when you get into an accident this will be evaluated on an individual basis in every situation.
“The limits have been made to provide a more equitable comparison between alcohol and other unsanctioned use of drugs, such as sleeping pills,” explains the researcher.
She is glad that the road law now includes explicit limits for such drugs that can be abused, but does not think this necessarily sanctions people to drive after using a drug, even though they have a prescription for it.
“Our conclusion is that you should be careful about driving a vehicle on the road after taking these medicines, whether you have a prescription or not,” she says.
Comprehensive data
The results of the study are based on a cross-check between two national registers, one for all prescriptions written in Norway and one for all traffic accidents on Norwegian roads.
The researchers used national identity numbers to find individuals who had purchased a prescribed medicine and been involved in a traffic accident.
The study comprised the entire Norwegian population and statistics covering nearly eight years.
“But we only know that they have bought the medicines, we have no evidence that they have actually used them,” says Gustavsen.
The research is based on numbers, not interviews. So there is no proof that the drugs are at blame or whether the increased likelihood of such accidents can be attributed to some other cause or situation relating to these persons.
Gustavsen says that a calculation has been made now that should make allowances for other possible causes among people buying the prescription drugs.
“When factoring this in we still see an increase linked to zopiclone.”
That isn’t all. While Gustavsen was working on her analysis, FHI conducted its own study of the relationship between Z-drugs and traffic accidents. It too found a correlation between road accidents and use of these pharmaceutical products.
Slower reactions
“These drugs are hypnotics and can have an effect on performance, like when you drink alcohol,” says the researcher.
Gustavsen conducted another study in connection with her PhD work, comparing zopiclone with alcohol, and found that their effects were analogous.
As with alcohol, zopiclone slowed down reactions.
-------------------------
Read the Norwegian version of this article at forskning.no
Translated by: Glenn Ostling