Why medicine can kill you
Allergic reactions to medicine are a serious side effect that can kill patients in rare cases. Researchers have now figured out why allergic reactions arise.
Abacavir is a drug used for treating HIV. Doctors have known for several years that patients with a specific type of cell (HLA-B*57:01) can suffer serious allergic reactions when they are treated with the drug. In the worst instances, the allergic reaction can kill the patient.
Doctors therefore check the patient’s tissue type before starting treatment. This has prevented patients suffering from these side-effects of the medicine.
So far, however, neither doctors nor researchers have known why people with cell type HLA-B*57:01 react so severely to Abacavir.
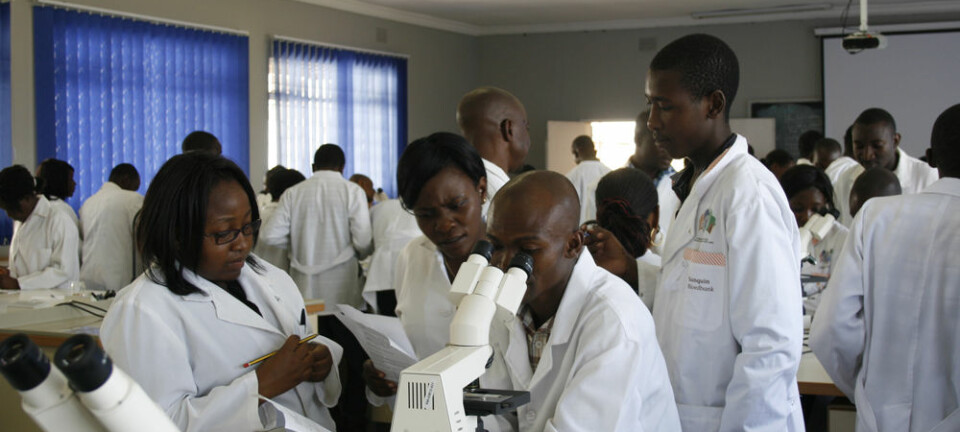
An international research team with Danish participation has now discovered that differences in the make-up of our immune defence are the reason why patients react so differently to Abacavir. The drug can actually change how the immune defence assesses its surroundings, so it believes that the body itself is a foreign object that must be eliminated.
We have found the molecular explanation to why the immune defence system reacts so severely to Abacavir treatment in precisely those patients with HLA-B*57:01, but not in other patients.
“This is a very severe allergic reaction in which patients can have bad skin rash, vomiting, diarrhoea and difficulties in breathing – and in the worst instances the reaction can kill them,” says Professor Søren Buus MD, of the Department of International Health, Immunology and Microbiology at the University of Copenhagen. “We have found the molecular explanation for the start of this reaction.”
Together with his international colleagues, Buus has just published these research results in the scientific journal PNAS.
Immune defence takes random samples
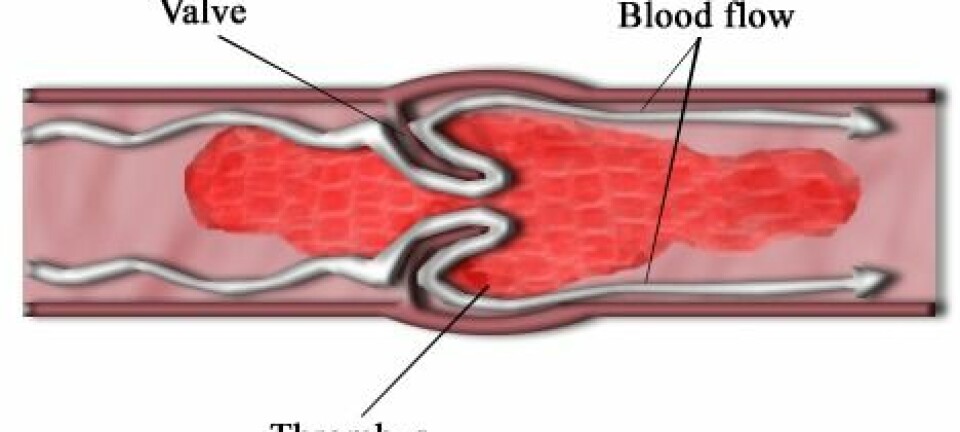
The T-cells are the most important cells in our immune defence system. They determine how the body defends itself against threats from e.g. bacteria and viruses.
But the T-cells do not work alone. They are assisted by human leukocyte antigens (HLAs), which, in a form of random sampling, take small samples from all of the body’s proteins and ‘show’ them to the T-cells.
We have discovered something new about the immune defence system.
The T-cells either approve the samples as having been produced by our body, or reject them as foreign objects – and tell the rest of the immune defence system that these ‘foreign’ proteins must be attacked and destroyed.
We have only a few of the thousands of HLAs that exist
In their work, the HLAs look for samples with certain characteristics. But searching for samples with certain characteristics also means that invasive micro-organisms will at some point find out what characteristics the HLAs are looking for, and the micro-organisms can then adapt to avoid discovery by the immune defence system.
To solve this problem, the immune defence has many thousands of HLAs with a sampling role, but they are distributed throughout the whole of mankind. Each person has only a few HLAs, but it’s very unlikely that two people have the exact same set of HLA samplers.
As the different HLA samplers search for different characteristics, no two individuals have immune defences searching for precisely the same samples.
In this way the immune defence system effectively prevents its samplers being discovered by invasive micro-organisms.
To prevent the T-cells reacting against an immune response to their own samples, they learn their target samples very early in their existence – so they know what is a threat and what isn’t.
Abacavir changes HLAs
The international research team’s results show that Abacavir can bind to the part of the HLA-B*57:01 cell that selects samples for review by the T-cells. This causes the HLA-B*57:01 cell to become interested in some samples that are completely different from those it is normally interested in.
When this happens, the immune defence system’s T-cells will start an immune response against all of the many new samples they review. This is why these patients have an allergic reaction to the drug.
“We have found the molecular explanation to why the immune defence system reacts so severely to Abacavir treatment in precisely those patients with HLA-B*57:01, but not in other patients,” says Buus.
Useful for drug makers
Although the problem of Abacavir treatment of patients with HLA-B*57:01 was solved a long time ago by deciding to check patients for HLA-B*57:01 before treating them with the HIV medicine, the new research results can be of great importance to the future development of drugs, according to the researchers.
The new knowledge can be used to change the chemical structure of Abacavir so the drug is no longer able to change the function of the HLA-B*57:01 cells. In that way the drug can be made to stick to its approved medical outcome.
The findings can also be used to understand how other drugs may possibly affect our immune defence.
“We have discovered something new about the immune defence system,” says Buus.
“This is useful knowledge for drug manufacturers in the future. One can imagine a situation where some medical trials have been stopped because a test person has reacted severely to the medicine. This could be because the person’s HLA samplers have simply been incompatible with precisely this drug. But the medicine can still be used to treat many other people as long as medical staff check the patients’ HLA samplers before they give the patients the medicine.”
--------------------------
Read this article in Danish at videnskab.dk
Translated by: Michael de Laine