Stopping treatment with blood-thinning drug can be fatal
Patients being treated with the blood-thinning medicine warfarin should be wary of breaking off their treatment as they then run a considerable risk of developing blood clots in the brain.
Millions of people around the world suffer from atrial fibrillation (fast, irregular heartbeat), and thousands of them are treated with the blood-thinning drug warfarin.
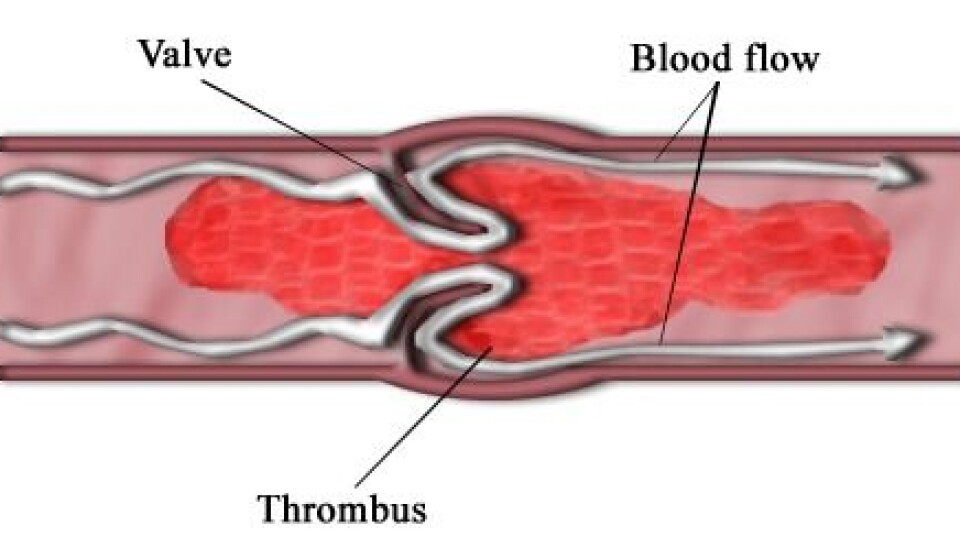
New research shows that while these patients benefit from their warfarin treatment, they risk getting a blood clot in their brain if they suddenly stop taking warfarin. A blood clot in the brain can result in paralysis in the body – and can be fatal.
“Our study shows that you should be extremely cautious in breaking off your warfarin treatment – you could lose your life,” says Christian Torp-Pedersen, a clinical professor at the Department of Surgery and Internal Medicine at Gentofte Hospital in Denmark, and a professor of cardiac medicine at the University of Copenhagen.
“You should be far more cautious than people are today, when both doctors and patients are a little too relaxed about stopping this treatment for atrial fibrillation.”
Data in several registers correlated
The researchers reached their conclusion after studying data in several Danish registers, including registers for medicinal product statistics and for causes of death. These contain details about the many Danish patients treated with warfarin over the years, their doses, when they run out of medicine and when they get more, their illnesses and causes of death.
Statistics over the number of blood clots for every 1,000 patients during and after treatment with warfarin showed a significant increase in the number of blood clots in patients shortly after the patients stopped taking the medicine.
“Our mission was to study what happens to patients who run out of medicine or who break off their treatment for other reasons,” says Torp-Pedersen. “By correlating the data in these registers we could see that these patients have a considerable risk for a blood clot in the brain after a break or at the end of their treatment.”
The number of blood clots rose by 300 percent during the first 90 days after the treatment ended, then fell gradually and stabilised after 180 days.
“When warfarin is taken, there will be about three blood clots in every hundred patient-years,” says the professor.
“That equals the risk run by patients without atrial fibrillation – which shows that the treatment is quite effective. But if the patients break off their treatment, the risk immediately rises to three times as many, to nine blood clots in every hundred patient-years, and then falls gradually again.”
Both doctors and patients have a responsibility
Torp-Pedersen says there are many reasons why patients stop taking the medicine: the atrial fibrillation stops and the patient’s heart rhythm returns to normal; to avoid the risk of bleeding, the patient stops the treatment temporarily ahead of dental work or surgery and for some days or weeks afterwards; and some patients cannot tolerate the medicine’s side effects.
“Breaks in the treatment because of dental work or surgery should be as short as possible,” he says. “Such patients could change to another blood-thinning drug such as heparin for a period. Unlike warfarin, which requires a slow reduction, heparin treatment can be started and stopped quickly. High-risk patients should change to heparin.”
Translated by: Michael de Laine
Scientific links
External links
- Christian Torp-Pedersen's profile
- About the Register of Medicinal Product Statistics
- About warfarin (Medline Plus)







