Scientists can predict risk of premature death 14 years in advance
One blood sample and some hi-tech analyses can reveal your risk of a premature death
Would you want to know if you were likely to die in the next 14 years? The results of a new study suggest that we may need to start seriously considering our answer to this question.
The new research can predict the long-term risk of developing severe infection, leading to hospitalisation and even death, based on the test results of a single blood sample.
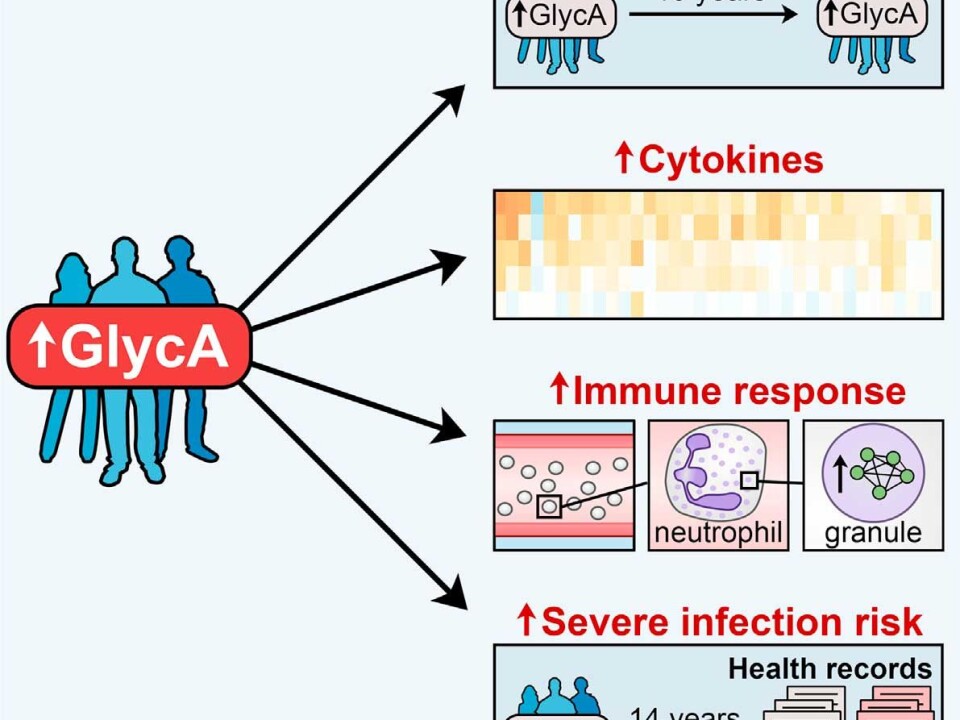
“People with a higher level of the biomarker GlycA in their blood sample had a much higher risk of infection, and even death, due to septicaemia and pneumonia, than those with lower levels over a 14-year period,” says co-author Johannes Kettunen, Head of Genetics, at the Computational Medicine Research Group, University of Oulu, Finland.
Kettunen and colleagues now hope to discover how to reduce people’s risk of premature death, as indicated by this GlycA molecule.
The new results are published in the scientific journal Cell Systems.
A molecular response to chronic infection
In the new study, Kettunen and colleagues analysed blood samples from more than 7,000 people--donated in 1997 as part of a large health survey organised by the Institute of Health and Welfare in Finland.
They were looking for GlycA, a molecule made up of a sugar bonded to a protein.
GlycA contains information on the abundance of a large group of similar molecules, which have important functions in the body. One of which is to modulate the immune system, and hence they can act as an early warning indicator for a range of diseases.
Kettunen and his team tracked the participants’ medical history through the Finnish national health registers to see what happened to them over the next fourteen years.
They found that people with elevated GlycA in their blood were not only more likely to suffer from severe infections like septicaemia and pneumonia, they were also more likely to suffer a premature death due to these infections.
“We saw that high levels of GlycA were stable in the body for more than ten years, and importantly, we saw that this was associated with specific molecular processes that indicated a state of chronic low-level inflammation and infection within the body,” says Kettunen.
A mechanism to explain GlycA’s predictive power
The new study identifies two key molecular processes that could explain GlycA’s predictive power.
First, in otherwise healthy individuals, elevated levels of GlycA corresponded to higher levels of a group of proteins--so-called cytokines. According to Kettunen, the body releases these proteins as anti-inflammatories to counteract inflammation.
Second, elevated GlycA also coincided with increased neutrophil activity--a type of white blood cell released in response to an infection.
“These two processes suggest that people’s immune system were in a continued state of response to chronic inflammation and infection somewhere in the body,” says Kettunen.
The long-term damage caused by this inflammation can render someone more susceptible to subsequent infections, and even death.
Colleague: a step closer to developing medical tests
Dr Krista Fischer, a biostatistician from the University of Tartu, Estonia, also studies the ability of GlycA to indicate health problems.
In an email to ScienceNordic she writes that the new research addresses “very important questions that may take us a step closer to the potential use of GlycA markers in medical diagnostics.”
She was not involved in the new research, but Fischer has worked with Kettunen on a previous project, where they first noticed an association between GlycA and premature death in otherwise healthy people.
“In this new study they’ve found strong evidence to support the theory that persistent chronic low-grade inflammation is a strong risk factor for common chronic diseases like cancer, cardiovascular diseases, and mortality,” writes Fischer, and notes that there is still much work to be done:
“As they point out in the paper, the underlying causes for such inflammation are not yet clear.”
Unethical to offer test when there is no treatment
When asked about how soon this test could be made available to the public, Kettunen is certain that it won’t be anytime soon.
“We’ve a lot of work to do before people can go to their doctors and ask for this test,” he says.
“Personally, I wouldn’t want to take the test, as I wouldn’t want to know the result. And in fact it would be unethical to offer it right now as there’s no treatments [available],” he says.
“The obvious question now is to find out what we can do to reduce people’s risk from these infections. So we need more research on the topic and ultimately to develop medication that could reduce the health risks indicated by high levels of GlycA,” says Kettunen.