
Mythbusting: There is no steroid “epidemic”
When you watch the news, it is evident that steroid use is a growing public health concern that demands a solution. But when you look at the numbers, there is little evidence to support that claim.
When the British reality tv celebrity, Spencer Matthews, appeared on the TV show Good Morning Britain (GMB) on July 13 2016 and talked openly about his previous and ‘mistaken’ use of anabolic steroids, the underlying theme was as clear as it was predictable: Steroid use is a threat to public health, and, more importantly, the number of users is increasing. Matthews, along with the general practitioner Dr. Hilary Jones, were invited to comment on the alleged explosion of young men using steroids for performance- and image-enhancing purposes.
In this steroid edition of GMB Investigates, needle exchanges and drug charities across the UK were contacted for information on the extent of the steroid problem. The investigation revealed that the number of steroid users accessing needle exchange clinics in South Wales had increased eightfold (from 269 to 2,161 visitors) between 2010 and 2015. They also reported that the use of steroids and image-enhancing drugs (SIEDs) in Cheshire and Merseyside in England were 20 percent higher than the year before, and that boys as young as 14 were taking steroids.
These apparently alarming results were quickly picked up by other news media who passed on the message that steroid use is on the rise, all arguing that it has now reached ’epidemic’ proportions. For instance, an article in the popular magazine Men’s Health set out to ’explore Britain’s anabolic appetite’, and claimed that ’… those who are taking them [steroids] are among a growing herd. In fact, they’re perfectly normal.’
That steroid use has become normalised among young people who simply want to look good is also a prevailing point of view outside the UK. In an article published by the Norwegian Policy Network on Alcohol and Drugs, the General Secretary of the network, Mina Gerhardsen, commented on a survey that revealed what she believed to be an increased use and acceptance of doping.
She stated that "the use and perception of doping are changing. While it was previously about having enormous muscles, more people are now using doping as a shortcut to achieve their dream body."
How the myth was established
The idea that the non-medical use of anabolic androgenic steroids (AAS) is increasing is frequently accepted without reservations by journalists driven by sensationalism, as witnessed above, as well as by academics seeking to justify their research. For instance, one study described the world population of AAS users as "growing" without substantiating the claim. Moreover, a Swedish doping scholar argued recently that the abuse of AAS is the second largest drug abuse problem in Sweden, surpassed only by alcohol abuse. But he did so without reference to any evidence other than experts’ opinions (including his own of course).
Unfortunately, claims like these are rarely questioned, although they are hardly ever substantiated by evidence. The idea that AAS use has escalated over the years seems to have acquired the status of ’common knowledge’ among some health professionals, drug use counsellors, and people in fitness and strength training environments.
Use of AAS does not seem to be on the rise
Notwithstanding how appealing the idea might be, it lacks evidence. In fact, when you look at the available evidence, it seems to support the opposite conclusion, namely that AAS use has remained relatively stable over the past two decades--perhaps even slightly decreasing since the turn of the century.
An increase in the number of AAS users visiting needle exchange services does not automatically indicate an increased prevalence of AAS. This would be like claiming that breast cancer is more prevalent because more women show up for mammagrohphy screening.
In that regard, the GMB investigation does not at all help to clarify the issue. The increased activity at needle exchange services could just as well be explained by more effective recruitment strategies and an increased awareness of AAS use among substance use workers. Likewise, it is difficult to conclude anything about drug use prevalence from statistics on drug seizures, since these numbers depend on several other factors such as allocation of resources and prioritization of tasks among the police and customs.
What do we know about the development of AAS use?
In fact, there are no convincing long-term data to support the idea that AAS use has increased during the past two decades. In a recent meta-analysis, the global lifetime prevalence of AAS use was estimated to 3,3 percent, with no significant difference between the two periods 1990-1999 (2,9 percent) and 2000-2013 (3,2 percent), and with no significant relationship between publication year and prevalence rate.
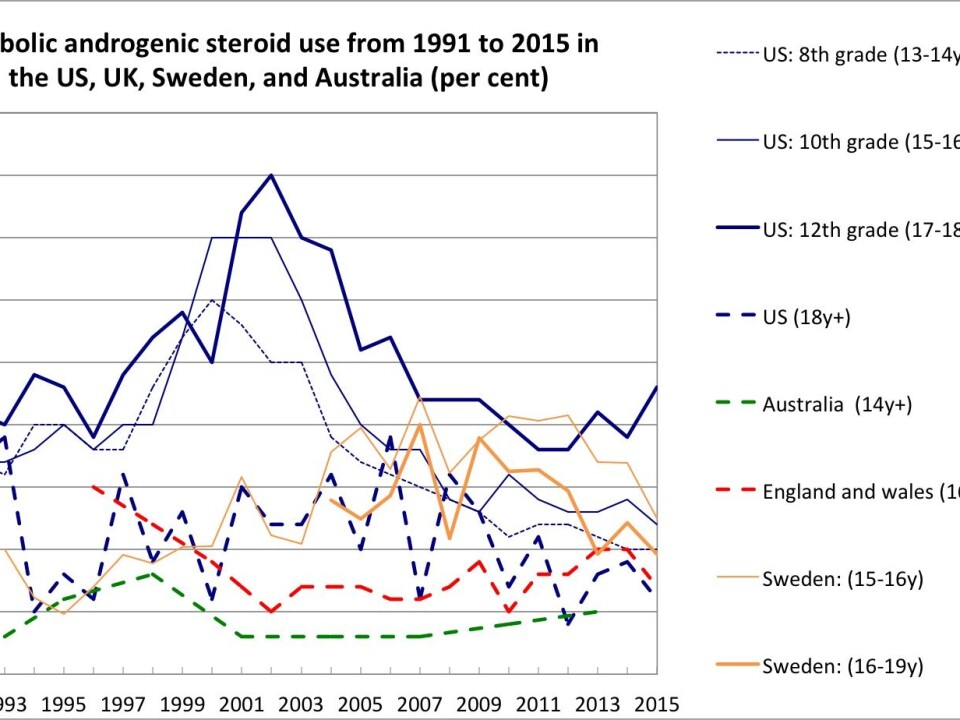
Since questions on AAS use are absent from most international drug surveys that have been conducted systematically on a long-term basis (e.g. UNODC’s World Drug Report and the European Drug Report), it is difficult to accurately determine how the global prevalence of AAS use has developed. However, there is one European and a some national surveys (primarily from the US, UK, Sweden and Australia) that have measured the prevalence of AAS use among different populations across a large enough time span – some since 1991 – to serve as qualified evidence for this question.
The European School Survey Project on Alcohol and Other Drugs (ESPAD) have published data on alcohol and drug use (including AAS) among European school children aged 15-16 every four years since 1995. The latest report was published October 20, 2016. According to this survey, the lifetime prevalence of AAS use has ranged from 0 to 5 percent in the participating European countries during the past two decades (1995-2015), but no clear cross-national patterns emerge from the data. Overall, the prevalence is low in the majority of the participating countries. In the last 20 years, it has typically oscillated between 0 and 2 percent, but whereas some countries (e.g. Bulgaria, Greece, Ireland and Poland) have experienced a slight increase, others (e.g. Croatia, Latvia, Slovenia and the UK) have experienced a decrease.
The results from the national drug surveys, most of which have been conducted more frequently than the ESPAD survey (e.g. every year or every second year), reveal a different and more consistent picture of the development of AAS use, as depicted in the figure below. Although there have been no drastic fluctuations in the use of AAS use between 1991 and 2015, a large minority of the surveys found that AAS use began to increase in the beginning of the 1990s, levelled off at the turn of the century, and then decreased in the following decades. Other surveys found little or no change at all, while only two surveys, one conducted among older adults aged 35-64 and one among school children in grades 9 through 12 in the period from 2009 to 2013, found an increase in the use of AAS.
Can we trust the data?
These data should of course be interpreted with caution. First, the use of AAS might in fact have increased despite data indicating the opposite. Most of the surveys used for the above figure are conducted in populations (e.g. school children and the general population) that are different from the typical AAS using population (mostly young, male gym users), and it is therefore possible that the use of AAS has increased in the latter population while having simultaneously decreased in the former two.
Considering the fact that the fitness industry is rapidly expanding, the absolute number of AAS users may therefore have increased if the prevalence rate in this population is assumed to have remained stable over the years (as witnessed above). For instance, since the number of commercial gym memberships in Denmark rose from approximately 550,000 in 2009 to around 810,000 in 2015, one can speculate that the number of people using AAS may have followed suit.
Also, false negative responses may result in an underestimation of the true prevalence. Such responses may be due to recall bias or more likely due to social desirability, a phenomenon well known in studies of doping in sport. On the other hand, false positive responses might explain differences in the opposite direction. For instance, in the 2011 ESPAD report, up to 3,1 percent answered that they had once taken the drug ’relevin,' which is a ’dummy drug’ that was used in the survey to highlight the risk of false positives.
Changes in the formulation of questions on AAS use can also influence how respondents understand and answer those questions. However, the surveys reporting to have changed their questions at some point in time only made minor revisions that are unlikely to have had any significant influence on the results.
Finally, there might be national variations in the prevalence of AAS use and how it has developed due to different social, cultural and institutional settings. However, the sparse evidence available at present does not allow for such comparisons between nations.
The discussion surrounding prevalence rates is not only of methodological relevance. Exaggerating the prevalence may be a problem in itself. A recent large-scale study among university and college students from seven EU countries demonstrated that perceived peer use of and attitudes toward alcohol predicted personal behaviour and attitudes. This has been shown to apply to the use of tobacco, cannabis, illicit substances and non-medical prescription stimulants. If these results can be generalised to AAS use, exaggerating the extent of the problem may actually contribute to increasing the number of users – an unintended consequence that will undeniably do more harm than good.
AAS use is a public health challenge
It is important to stress that we are not trying to downplay the public health issues related to AAS use. Since it was not before the beginning of the 1980s that AAS use became widespread outside elite sport, we have yet to witness the long-term medical consequenses among former and current AAS users. However, it is widely acknowledged that there are a wide range of adverse health consequences associated with AAS use such as cardiovascular disease, suppression of the hypothalamic-pituitary-testicular (HPT) function, depression and dependence.
Neither are we claiming that AAS use is a phenomenon that belongs to the past. Although available evidence does not support the claim that steroid use has escalated over the years, a recent study from the UK indicates that steroid use has become a larger challenge to public health during the past two decades. This is evidenced by an increase in the number of steroid users visiting needle and syringe programmes (NSPs) in the period from 1995 to 2015, and a simultaneous explosion in the total number of dispensed syringes (from 14.293 to 139.956) as well as in the number of dispensed syringes per individual (from 26 to 57).
Thus, the non-medical use of AAS clearly poses a challenge to public health. Policy makers, health professionals and people working with the prevention of substance use should take the physical, psychological and social consequences of AAS use seriously. But until solid evidence becomes available, the idea that steroid use is an ’epidemic on the rise’ remains nothing more than a myth.
---------------
This article is an edited version of an article that first appeared on the website of the International Network for Doping Research.






