Many women needlessly take cholesterol-lowering drugs
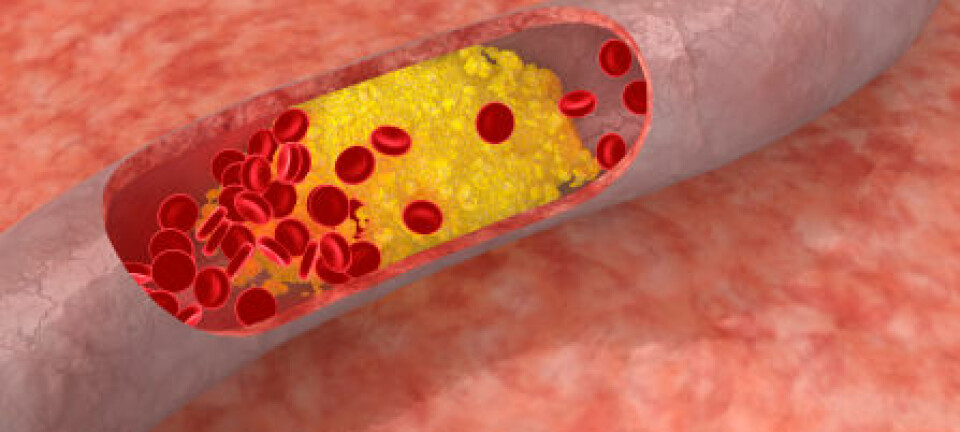
More than half of middle-aged women who take cholesterol-lowering medicines called 'statins' have neither cardiovascular disease or diabetes, shows new research.
Statins are commonly prescribed as a 'primary prevention' against cardiovascular disease in high-risk individuals even if they don’t already suffer from cardiovascular disease or type-2 diabetes, and they are recommended as a lifelong therapy in people over 75 years.
But a new study questions their efficacy and raises concern that women over the age of 50 are needlessly prescribed statins to lower cholesterol.
“Cholesterol levels need to be lowered if they are 'elevated' but I think there is a tendency to over-treat, which is worrying," says co-author Helle Wallach Kildemoes, Associate Professor at the Department of Pharmacy at the University of Copenhagen, Denmark.
The study is published in the Journal of Evaluation in Clinical Practice.
No need to take medication if you are healthy
In the new study, scientists looked at the use of statins in nearly 4.5 million Danes between 2000 and 2010, during which the number of people prescribed statin therapy increased more than tenfold.
To find out why, they examined records of hospital admissions and the use of prescription drugs. It is the first time that researchers have analysed the reasons for prescribing these cholesterol-lowering drugs.
They saw that 60 per cent of the 50 to 60 year-old women were prescribed medication even when they did not suffer from heart disease or diabetes.
"Treatment is given to people who are actually healthy, without understanding the effects. If you're healthy, I don’t think there is any reason to take [this] medication," says Mats Lindberg, a consultant in rheumatology and co-founder of the network Physicians Without Sponsors, in Denmark.
Kildemoes agrees.
"We don’t know if they has a preventive effect, and at the same time statins have side effects--muscle pain. It’s a problem,” she says.
Lindberg recommends that patients should monitor their cholesterol unless there are specific problems related to a family history of heart attacks or cardiovascular disease.
"It makes sense to take statins if, for example, you’ve had a heart attack or type-2 diabetes, otherwise preventive treatment is questionable," he says.
The drug has little effect
The preventive effect of the drug in healthy people is uncertain.
A previous study showed that statins have a limited effect in lowering cholesterol, even if you have had blood clots, cardiovascular disease, or diabetes.
In this study, statins prolonged the life of patients by 5 to 27 days after five years of treatment.
Professor Jesper Hallas, from the Department of Pharmacology at the University of Southern Denmark, was a co-author on this earlier study.
"Our study showed that the average delay of death is very small. It's just a few days,” he says. “So it might be good to know, for those who have side effects, that the longevity effect is quite small," says Hallas.
But he stresses that the efficacy of statins in preventing blood clots, for example, is well documented and can prolong life by a few days.
"But to start taking this medicine at 80 probably isn’t very rewarding,” he says. “If I was in my 70s and got a blood clot, then I would take statins, but I would quit if I suffered side effects, says Hallas.
Elderly are over-medicated
Despite the very limited effect on longevity, more and more elderly people are receiving statins.
In 2000, two to three per cent of elderly people aged 75 to 84 took statins. But by 2010 this had risen to more than a third, and it was slightly higher for men than for women.
"It’s problematic because there is no evidence that the drug has a beneficial effect in the elderly. Elderly people often take many different types of medication and they are more sensitive to the side effects," says Kildemoes.
Both Lindberg and Hallas believe that there is too much focus on the side-effects of statins, which, they say, are very limited and well documented. However Lindberg believes we should pay more attention to side effects in the elderly.
"Doctors must pay more attention to muscle pain and weakness in the elderly, who receive statins," says Lindberg.
He thinks that doctors should reduce the dose in the most elderly patients and stop treatment when it is no longer useful as a preventive treatment.
"There are studies and guidelines on when to start medication. These studies come from the pharmaceutical industry. But there are no studies on when to stop the medication," he says.
--------------
Read the Danish version of this story on Videnskab.dk
Translated by: Catherine Jex
Scientific links
- Statin prescribing according to gender, age and indication: what about the benefit–risk balance?, Journal of Evaluation in Clinical Practice (2015), doi: 10.1111/jep.12462
- The effect of statins on average survival in randomised trials, an analysis of end point postponement, BMJ (2015), doi: 10.1136/bmjopen-2014-007118