Immunotherapy does not work for everyone
New research reveals why some patients do not benefit from immunotherapy treatments.
Scientists are one step closer to understanding why immunotherapy is an effective treatment for some cancer patients but not for others.
Immunotherapy is a new type of treatment that is touted by some as a breakthrough in the fight against cancer. It uses the body's own immune system to attack cancer cells. But the treatment is expensive, it has many side effects, and in some patients it has virtually no effect.
Now scientists have discovered how immunotherapy activates the immune system to recognise and destroy cancer cells in some patients but not in others. It seems that the immune system can only recognise cancer cells that have particular genetic mutations.
"It's very big news, which gives us a much better understanding of how immunotherapy works," says Marco Donia from the Centre for Cancer Immunotherapy (CCIT) at Herlev Hospital, Denmark, who was not involved in the new research.
"It's certainly an exciting and important discovery. Immunotherapy is a very expensive treatment, which only has an effect on some patients. It’s vital that we have the tools to see which patients will benefit from treatment and which ones won’t," says Professor Ulrik Lassen from the oncology department at the University of Copenhagen Hospital, Denmark. He was not involved in the new research.
The immune system recognises particular genetic mutations
In the new study, which is published in the journal Science, scientists show that the success of treatment depends on the composition of the patient’s genetic mutations in their cancer cells.
Only then, can the body's immune system recognise and attack the cancer when the patient is receiving immunotherapy.
Cancer tumours are like trees
These mutations are found in what is called the cancer cell strain, explains co-author Sine Reker Hadrup, associate professor in the department of immunology and vaccinations at the National Veterinary Institute, Technical University of Denmark (DTU).
She compares the growth of cancer tumours with a tree. As it grows, the tumour branches out and develops new genetic mutations.
The original gene mutations of the strain are present in all tumour cells. But as the tumour grows and develops more branches with more mutations, the immune system finds it harder to recognise the cells as foreign bodies.
"We have developed technologies that show what the immune system recognises. Cancer cells exhibit some of their mutations on the cell surface and in this study we measured, which of these mutations, the immune system is able to recognise and attack when activated by immunotherapy," says Hadrup.
"We’ve examined cancer tumours in a few patients and we can see that their immune systems exclusively binds to the mutations that sits in the stem of the cancer cell," she says.
Hadrup’s conclusions are supported by another study that is based on the genetic makeup of hundreds of cancer patients' tumours.
"Immunotherapy has a poor effect in patients with more genetic mutations in the branches of the cancer tumour than in the stem," says Hadrup.
Chemo may reduce the efficacy of immunotherapy
Immunotherapy is approved for patients with lung, kidney, and skin cancer. But so far, immunotherapy is only used as an initial form of treatment for skin cancer. Chemotherapy or radiation therapies are still recommended as the initial treatment for lung and kidney cancers.
But the new study suggests that this might be a bad idea, says Lassen.
Previous research has shown that chemotherapy and radiation therapy can promote the development of new types of genetic mutations in cancer cells, so-called sub-clones. And these sub-clones reduce the efficacy of immunotherapy, he says.
"We know that chemotherapy and radiation therapy can cause DNA damage and help to stimulate the development of sub-clones. In this study, we see that the immune system has difficulty recognising cancer cells if there is a large variety of sub-clones in cell mutations. It thus appears that chemo and radiation therapy can help to reduce the effect of immunotherapy in some cases," says Lassen.
No immediate change to treatment
But even though the new research outlines how to identify patients who benefit most from immunotherapy, Donia does not expect to see these techniques in use in hospitals anytime soon.
"It gives us a greater understanding of how immunotherapy works, but it doesn’t change our treatment strategy [right now]," he says.
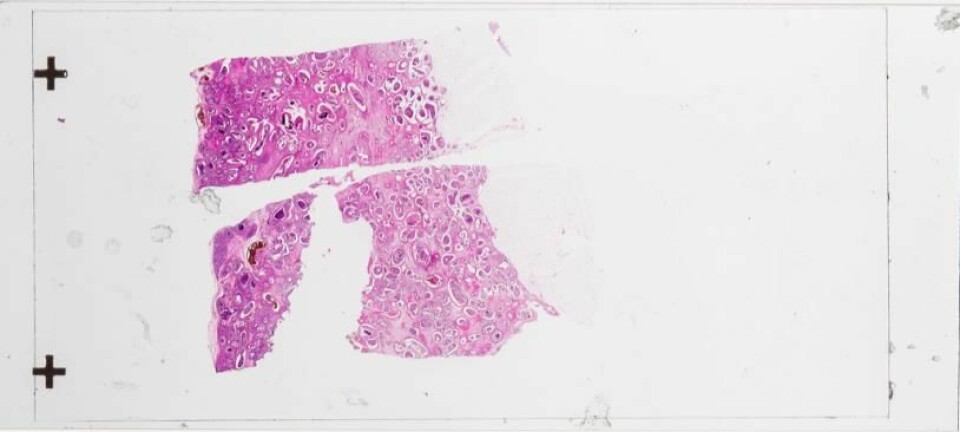
"We need more studies, and if we are to use this in hospitals to predict which patients will benefit from immunotherapy, then we have to have the equipment to make tissue samples and DNA analyses of the tumours," says Donia.
-------------
Read the Danish version of this story on Videnskab.dk
Translated by: Catherine Jex