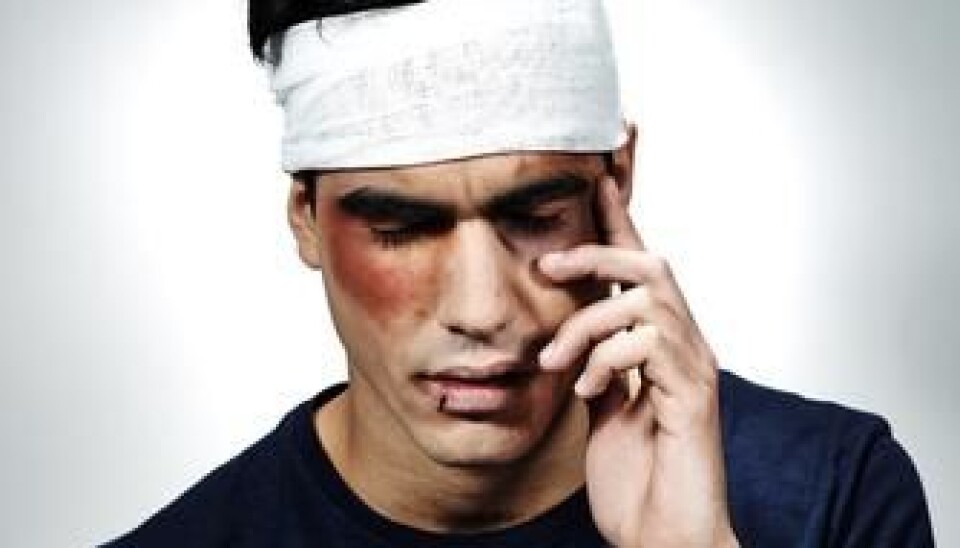
Head injury can cause mental illness
If you suffer a head trauma, your risk of developing certain mental disorders increases significantly – in some cases by more than 400 percent, new study reveals.
Danish scientists have studied the link between head traumas such as concussion and skull fracture and the subsequent risk of developing mental disorders.
They found that head injuries can increase the risk of developing certain mental disorders by up to 439 percent.
“I am quite surprised by our findings. I had expected to see a correlation, but it is stronger than I had expected,” says Sonja Orlovska, MD, of the Psychiatric Centre Copenhagen.
She is the lead author of the new study, published in the American Journal of Psychiatry.
Largest study to date
This is the largest study of its kind. It is a national register study based on all Danes born between 1977 and 2000 – totalling 1.4 million people – who were followed up to 2010.
I am quite surprised by our findings. I had expected to see a correlation, but it is stronger than I had expected.
In this period, 113,906 of them had been admitted to hospital with a head injury. Four percent of these were subsequently diagnosed with a mental disorder.
The researchers looked at the following disorders: depression, schizophrenia, bipolar disorder and so-called organic mental disorders (a form of decreased mental function due to a medical or physical disease, rather than a psychiatric illness).
By comparing the injured people’s risk of developing the disorders with the rest of the study population, they found that those with head injuries were:
- 65 percent more likely to be diagnosed with schizophrenia.
- 59 percent more likely to develop a depression.
- 28 percent more likely to be diagnosed with bipolar disorder.
- 439 percent more likely to suffer from organic mental disorders.
The greatest risk of developing a mental disorder is in the first year after suffering head trauma, but even after 15 years there was a significantly increased risk.
A chicken-and-egg situation
Orlovska is particularly surprised to see that there is a significant correlation between head trauma and mental disorders even after adjusting the results for a known confounding factor:
”We know, for instance, that depression leads to reduced power of concentration, and that the early phase of schizophrenia is associated with an increased susceptibility to accidents. So which came first: the disorder or the head trauma? Most of the previous research has failed to address this, but we have tried to work around the problem,” she says.
The researchers examined whether people who had been admitted to hospital with a broken toe or similar injuries also have a significantly greater risk of developing a mental disorder. It turned out that they do, but here the risk was much lower than with head traumas.
They found that, for example, a person who enters a hospital emergency room with a broken arm has a 16-percent greater risk of being diagnosed with schizophrenia, whereas for a person who has suffered head trauma, the risk increases by 65 percent.
”We adjusted for this effect and found that regarding schizophrenia, depression and the organic mental disorders there is still a significantly increased risk of developing a mental disorder after suffering head trauma,” says Orlovska.
The researchers also adjusted for a family history of mental disorders, but this did not change the results significantly.
Inflammation and disturbed neurotransmitters may be the cause
Although there is no definite explanation to the correlation between head injuries and the subsequent development of mental disorders, Orlovska believes there are several possible explanations:
- Animal studies have shown that a head trauma typically causes inflammation in the brain, and this increases the risk of psychological symptoms.
- Head injuries can destroy an area of the brain, and this damage can lead to the development of a mental disorder that is associated with the area in question.
- A more diffuse injury such as a concussion can affect the neurotransmitters that the brain uses to communicate between various parts of the nervous system, and this disrupted balance is associated with the development of mental disorders.
- The head injury may have occurred in connection with a traumatic accident, and perhaps it is the psychological and emotional reaction to the trauma that triggers the mental disorder. The loss of bodily functions or abilities after an accident with head trauma may also affect the psyche so that the patient develops a mental disorder.
Study may lead to improved treatment
Orlovska hopes that the new findings may lead to a better understanding of the causes of mental illness.
Knowing about the increased risk from head traumas may also help doctors to detect mental disorders at an earlier stage in their development.
----------------------
Read the Danish version of this article at videnskab.dk