Genetic test identifies “high risk” lymphatic cancer patients
Patients with mantle cell lymphoma are more likely to relapse if they carry mutations in the cancer gene, TP53. The results could help provide more targeted treatments for this “high risk” group.
Around 1,500 people in Denmark are diagnosed with lymphatic cancer each year. A small sub-group (70 to 80 people) develop a rare and aggressive type of lymphatic cancer, known as mantle cell lymphoma (MCL).
The prognosis for MCL patients has markedly improved in the past 10 years and research shows that most patients respond well to standard treatment.
Unfortunately, this same research also shows that a small sub-group of patients do not respond to treatment: They relapse early and have a high mortality rate.
In a new study, we show how a new gene test can identify the majority of these “high risk patients” when they are first diagnosed with the cancer, paving the way for more effective treatments for this group.

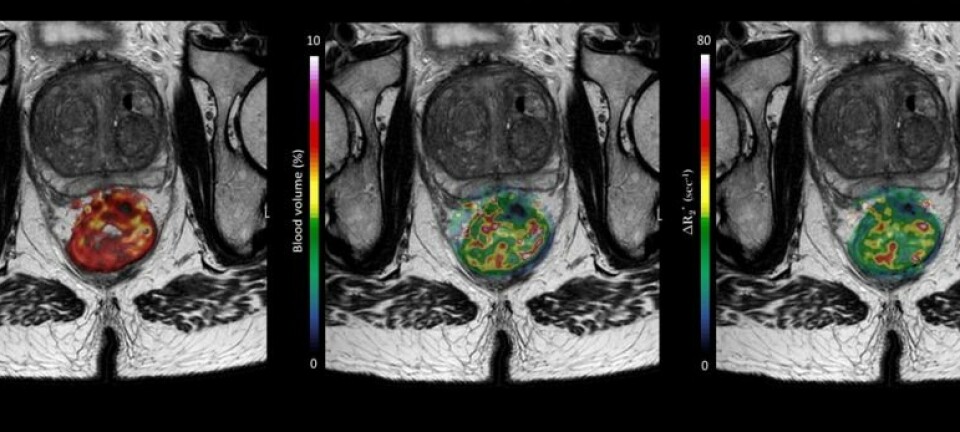
Read More: Blood test detects susceptibility to aggressive rectal cancer
The TP53 cancer gene
We looked for mutations in the TP53 gene—a well known gene that is found in many different types of cancer.
Normally, the gene’s job is to protect the cell against DNA synthesis errors when the cells divide.
When TP53 records a mistake in the DNA, it sends out a signal that the cell division should stop and that the mistake should be repaired before cell division can start again.
If the mistake cannot be repaired, then TP53 sends a signal that the cell should die.
This prevents the cells accumulating errors in the DNA, which can lead to a vicious transformation into, for example, a cancer cell.
But when the TP53 gene is mutated in a cancer these protective mechanisms are inhibited, the cell may accumulate DNA-errors, increase the rate of cell division and become resistant to “death”-signals.
Read More: Should I really stop taking the pill to prevent breast cancer?
Safe method identifies high risk patients
The Nordic Mantle Cell Lymphoma Group (covering Denmark, Norway, Sweden, and Finland) has been at the forefront of improving treatment of MCL.
We analysed patient samples collected between 2000 and 2009 and stored at Rigshospitalet in Copenhagen, Denmark, under the leadership of Professor Kirsten Grønbæk from the Department of Haematology at Rigshospitalet.
Using a well-known test targeting the TP53 gene we were able to identify the group of high risk patients.
Eleven per cent of all MCL patients harboured a mutated variant of the TP53 gene, and hereof 55 per cent had relapsed and died only two years after treatment. Conversely, patients with unaffected TP53 gene experienced long term remissions, and more than half were still alive and in remission 12 years after treatment.
Read More: Genes for cold climates linked to cancer?
New treatment for patients with mutated TP53
The test divides patients into two groups with very different outcomes and may have significant implications for treatment of MCL, globally.
The prognosis for patients with unmutated TP53 is generally good with the current standard-of-care, but clearly patients with mutated TP53 are in need of new therapeutic approaches.
In another new Nordic study for the treatment of recurrent MCL, we studied a combined treatment that targeted biological signal pathways in the cells instead of using chemotherapy.
Results so far are promising, and we see no difference in the rate of relapse between the two groups of normal and mutated TP53, respectively.
Thus, the preliminary results of this trial suggest, that these new drugs could represent a more effective alternative for high risk patients with the TP53 mutation in the future, even at the first stage of treatment.
The MCL project is supported by the Independent Research Fund Denmark and the Rigshospital Research Fund.
---------------
Read this article in Danish at ForskerZonen, part of Videnskab.dk
Translated by: Catherine Jex
Scientific links
- Eskelund, C.W., Dahl, C., Hansen, J.W., Westman, M., Kolstad, A., Pedersen, L.B., Montano-Almendras, C.P., Husby, S., Freiburghaus, C., Ek, S., Pedersen, A., Niemann, C., Räty, R., Brown, P., Geisler, C.H., Andersen, M.K., Guldberg, P., Jerkeman, M. & Grø
- Eskelund, C.W., Kolstad, A., Jerkeman, M., R??ty, R., Laurell, A., Eloranta, S., Smedby, K.E., Husby, S., Pedersen, L.B., Andersen, N.S., Eriksson, M., Kimby, E., Bentzen, H., Kuittinen, O., Lauritzsen, G.F., Nilsson-Ehle, H., Ralfki??r, E., Ehinger, M.,
- Jerkeman, M., Hutchings, M., Räty, R., Wader, K.F., Laurell, A., Kuitunen, H., Toldbod, H., Pedersen, L.B., Eskelund, C.W., Grønbæk, K., Niemann, C.U., Geisler, C.H. & Kolstad, A. (2016) Ibrutinib-Lenalidomide-Rituximab in Patients with Relapsed/Refractor
- Olivier, M., Hollstein, M. & Hainaut, P. (2010) TP53 mutations in human cancers: origins, consequences, and clinical use. Cold Spring Harb Perspect Biol, 2, a001008