Breaking through brain’s defence to let in meds
The mystical blood-brain barrier protects the brain like a sentry, making it difficult to get through with vital life-saving medications. Uppsala Professor Christer Betsholtz is trying to find the key needed to enter.
The blood-brain barrier protects the brain from harmful intruders. It guards the headquarters as a constant and reliable sentry.
It is a semi-permeable membrane which ensures that only the right substances pass through the blood and into our brain and central nervous system. Nasty things like bacteria and toxins that can be found in the intestines – harmful to the brain – are denied entrance through any “doorways”.
We can be grateful. But on the other hand, modern medicine has reached a point where medications could be developed which might treat brain diseases like Alzheimer’s – if only the medications were given a free pass.
That poses a problem, because this blood-brain barrier is such a strong protector.
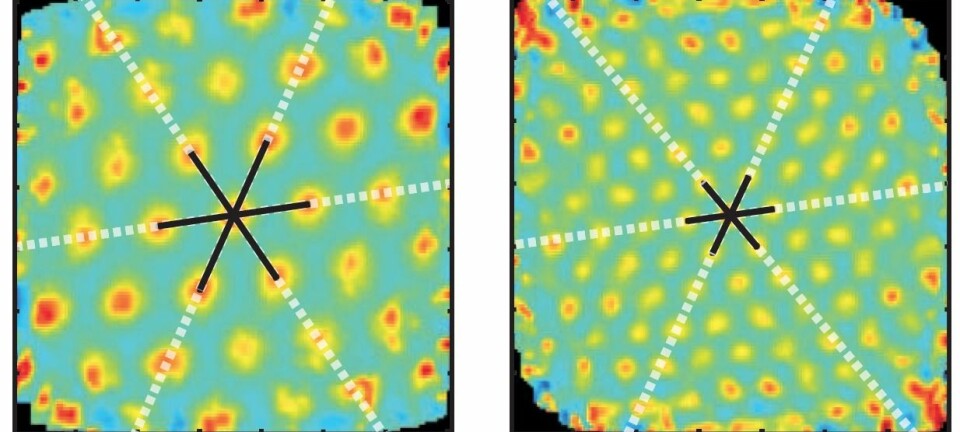
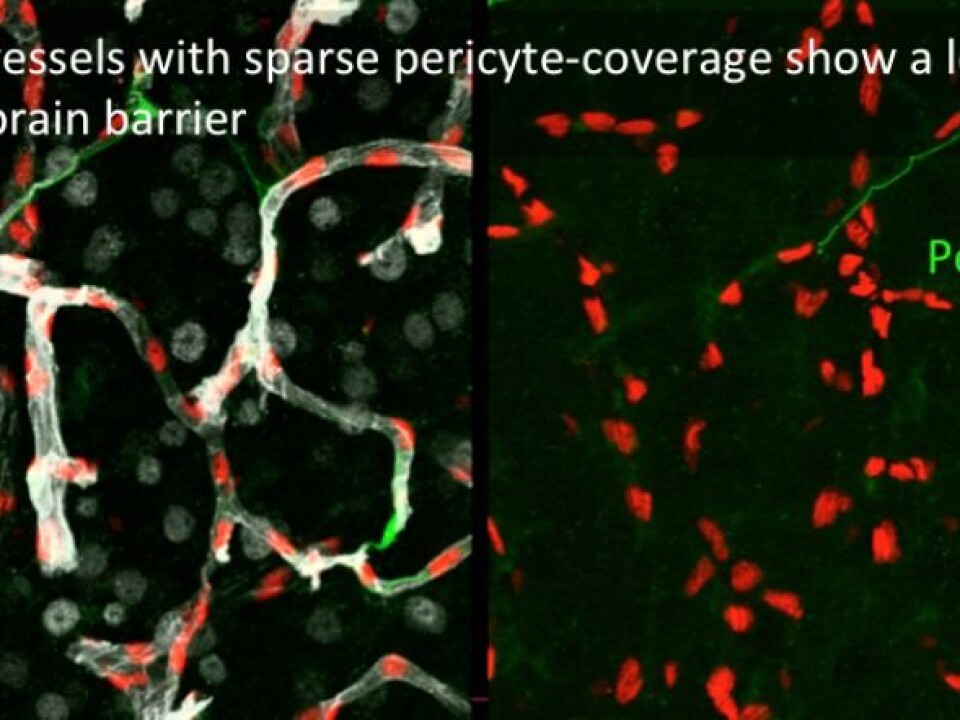
![Betsholtz and colleagues found that the capillaries [tiniest arteries] in the brain with a normal number of pericytes had an intact blood-brain barrier. (Photo: Dr Maarja Andaloussi Mäe)](https://image.sciencenordic.com/1447015.webp?imageId=1447015&width=960&height=720&format=jpg)
What if we could coax it to slack off a little – just for certain substances and a limited space of time?
Modest cells key to creating blood vessels
This is what Christer Betsholtz has researched. He is a professor in vascular and tumour biology at the University of Uppsala. Recently he was declared the main winner of the Anders Jahre’s Award 2017 for his “ground-breaking contribution toward our understanding of how the networks of tiny blood vessels are formed and function, and the medical significance of this”.
“Betsholtz’s work is pioneering because it gives us a new view of how blood vessels and the capillary network are formed, and how the flow of blood through the blood vessels is regulated,” says the head of the Jahre’s Award jury, Harald A. Stenmark.
The major keys toward opening the equivalent of a door through the blood-brain barrier just a crack, in certain cases, has been small cells called pericytes. These are found in the outer walls of capillaries.
Betsholtz started research on these in the mid-1990s. Until then, all the years since the 1800s when they were first discovered, nobody knew much about these cells.
“This opened up research about pericytes. They turned out to be something other than anonymous structures in the walls of capillaries. We found out what their function is,” says Betsholtz.
Leaks without pericytes
He and his colleagues were actually researching cancer development in mice which they had manipulated with a certain substance – a growth factor. What they discovered came as an utter surprise: The mice turned out to lack pericytes.
The researchers did not yet know why. But in the following years they forged ahead with this research and in 1997 they published a study with several of the answers.
“We found that pericytes rely on this growth factor to develop. They actually contain receivers for this growth factor.”
What the lack of pericytes led to in the mice proved how fundamental and vital these cells are for the blood vessels and thus for life and health:
“The capillaries of the mice had leaks and were immature,” explains Betsholtz.
Discovered a secret “passage”
Betsholtz and colleagues had heard about a theory that the pericytes could be important contributors to the blood-brain barrier. This sounded reasonable as these cells are so important to the proper development of capillaries.
They decided to research this on mice that partly lacked pericytes. Would the scantiness of these cells cause a partly weakened barrier which in turn would allow substances to pass from the blood to a brain – and importantly, a brain needing medications that would be administered through the bloodstream?
The notion that it could be safe for the brain to lower its guard in this way had been inconceivable.
“It was presumed that this was fatal,” said Betsholtz.
The mice they tested did indeed have an impaired blood-brain barrier. The web of tight capillaries had opened up, just a crack, so to speak. And the mice were still alive and well.
The researchers could now show which routes in the circulatory system led to this opening in the mice. They could transport antibodies through this barrier and into the brain. This could turn out to be an inroad for treating Alzheimer’s.
Enthusiasm
One of the many who think the prize given to Christer Betsholtz is well deserved is Erlend Arnulf Nagelhus at the Institute of Basic Medical Sciences at the University of Oslo (UiO). He too conducts research on the obstinate blood-brain barrier.
“For starters, Betsholtz’s thrilling results have created enthusiasm for research on pericytes and the blood-brain barrier. Betsholtz’s research has also paved the way for the perception that an intact interplay among different types of cells is vital for the blood-brain barrier’s function,” says Nagelhus.
If we could learn how pericytes regulate the barrier we can hopefully manage to develop new medicines to treat diseases of the central nervous system,” says the jury chairman Harald Stenmark.
“Betsholtz has also found that capillaries around malignant tumours often lack pericytes and the tumours promote proliferation by disturbing the interplay between capillaries and pericytes. This facilitates the passage of cancer cells through the blood vessel walls. It is something we can make use of in future treatment of cancer,” he says.
Knowledge is still shallow
Despite such discoveries, the prize winner says scientists have not made nearly enough headway towards finding out how to use these narrow doorways into the brain for treating diseases.
Most medications consist of small molecules which are lipid solvent. They dissolve in fats. These are molecules that this defence system recognises as adversaries because they are like something bacteria make.
But the researchers have managed to attach certain antibodies to hormones that do have access to the brain, for example the hormone transferrin. This is an iron-transport protein in blood serum. It hauls iron in through the barrier with antibodies as passengers.
“This is on the basic research level, but it might impact a disease such as Alzheimer’s. I’m optimistic – this is the first route that researchers have seriously been able to test.”
“Nevertheless, we have terribly much we don’t know and the depth of our knowledge is not all that deep.”
Barrier genes
Betsholtz and his research partners are now also working on an overview of genes linked to the cells in the blood-brain barrier.
“You could say we are trying to create a sort of reference work which I hope everyone could use in their research in years to come.”
He emphasises that the road ahead needs to plough deeper in analysing how the barrier and its cells work.
“To make headway in research we need to continue with basic research. We will also collaborate with researchers on brain tumours and others who specialise in Alzheimer’s research. Maybe we can attain a better understanding of how pericytes play a role here too,” says Christer Betsholtz.
-------------------------------------
Read the Norwegian version of this article at forskning.no
Translated by: Glenn Ostling